Category: Neuroscience
Scientists Construct First Detailed Map of How the Brain Organizes Everything We See

Our eyes may be our window to the world, but how do we make sense of the thousands of images that flood our retinas each day? Scientists at the University of California, Berkeley, have found that the brain is wired to put in order all the categories of objects and actions that we see. They have created the first interactive map of how the brain organizes these groupings.
The result — achieved through computational models of brain imaging data collected while the subjects watched hours of movie clips — is what researchers call “a continuous semantic space.”
“Our methods open a door that will quickly lead to a more complete and detailed understanding of how the brain is organized. Already, our online brain viewer appears to provide the most detailed look ever at the visual function and organization of a single human brain,” said Alexander Huth, a doctoral student in neuroscience at UC Berkeley and lead author of the study published Dec. 19 in the journal Neuron.
A clearer understanding of how the brain organizes visual input can help with the medical diagnosis and treatment of brain disorders. These findings may also be used to create brain-machine interfaces, particularly for facial and other image recognition systems. Among other things, they could improve a grocery store self-checkout system’s ability to recognize different kinds of merchandise.
“Our discovery suggests that brain scans could soon be used to label an image that someone is seeing, and may also help teach computers how to better recognize images,” said Huth.
It has long been thought that each category of object or action humans see — people, animals, vehicles, household appliances and movements — is represented in a separate region of the visual cortex. In this latest study, UC Berkeley researchers found that these categories are actually represented in highly organized, overlapping maps that cover as much as 20 percent of the brain, including the somatosensory and frontal cortices.
To conduct the experiment, the brain activity of five researchers was recorded via functional Magnetic Resonance Imaging (fMRI) as they each watched two hours of movie clips. The brain scans simultaneously measured blood flow in thousands of locations across the brain.
Researchers then used regularized linear regression analysis, which finds correlations in data, to build a model showing how each of the roughly 30,000 locations in the cortex responded to each of the 1,700 categories of objects and actions seen in the movie clips. Next, they used principal components analysis, a statistical method that can summarize large data sets, to find the “semantic space” that was common to all the study subjects.
The results are presented in multicolored, multidimensional maps showing the more than 1,700 visual categories and their relationships to one another. Categories that activate the same brain areas have similar colors. For example, humans are green, animals are yellow, vehicles are pink and violet and buildings are blue.
“Using the semantic space as a visualization tool, we immediately saw that categories are represented in these incredibly intricate maps that cover much more of the brain than we expected,” Huth said.
Other co-authors of the study are UC Berkeley neuroscientists Shinji Nishimoto, An T. Vu and Jack Gallant.
Journal Reference:
1.Alexander G. Huth, Shinji Nishimoto, An T. Vu, Jack L. Gallant. A Continuous Semantic Space Describes the Representation of Thousands of Object and Action Categories across the Human Brain. Neuron, 2012; 76 (6): 1210 DOI: 10.1016/j.neuron.2012.10.014
http://www.sciencedaily.com/releases/2012/12/121219142257.htm
The brain’s natural valium

Hitting the wall in the middle of a busy work day is nothing unusual, and a caffeine jolt is all it takes to snap most of us back into action. But people with certain sleep disorders battle a powerful urge to doze throughout the day, even after sleeping 10 hours or more at night. For them, caffeine doesn’t touch the problem, and more potent prescription stimulants aren’t much better. Now, a study with a small group of patients suggests that their condition may have a surprising source: a naturally occurring compound that works on the brain much like the key ingredients in chill pills such as Valium and Xanax.
The condition is known as primary hypersomnia, and it differs from the better known sleep disorder narcolepsy in that patients tend to have more persistent daytime sleepiness instead of sudden “sleep attacks.” The unknown cause and lack of treatment for primary hypersomnia has long frustrated David Rye, a neurologist at Emory University in Atlanta. “A third of our patients are on disability,” he says, “and these are 20- and 30-year-old people.”
Rye and colleagues began the new study with a hunch about what was going on. Several drugs used to treat insomnia promote sleep by targeting receptors for GABA, a neurotransmitter that dampens neural activity. Rye hypothesized that his hypersomnia patients might have some unknown compound in their brains that does something similar, enhancing the activity of so-called GABAA receptors. To try to find this mystery compound, he and his colleagues performed spinal taps on 32 hypersomnia patients and collected cerebrospinal fluid (CSF), the liquid that bathes and insulates the brain and spinal cord. Then they added the patients’ CSF to cells genetically engineered to produce GABAA receptors, and looked for tiny electric currents that would indicate that the receptors had been activated.
In that first pass, nothing happened. However, when the researchers added the CSF and a bit of GABA to the cells, they saw an electrical response that was nearly twice as big as that caused by GABA alone. All of this suggests that the patients’ CSF doesn’t activate GABAA receptors directly, but it does make the receptors almost twice as sensitive to GABA, the researchers report today in Science Translational Medicine. This effect is similar to that of drugs called benzodiazepines, the active ingredients in antianxiety drugs such as Valium. It did not occur when the researchers treated the cells with CSF from people with normal sleep patterns.
Follow-up experiments suggested that the soporific compound in the patients’ CSF is a peptide or small protein, presumably made by the brain, but otherwise its identity remains a mystery.
The idea that endogenous benzodiazepinelike compounds could cause hypersomnia was proposed in the early 1990s by Elio Lugaresi, a pioneering Italian sleep clinician, says Clifford Saper, a neuroscientist at Harvard Medical School in Boston. But several of Lugaresi’s patients later turned out to be taking benzodiazepines, which undermined his argument, and the idea fell out of favor. Saper says the new work makes a “pretty strong case.”
Based on these results, Rye and his colleagues designed a pilot study with seven patients using a drug called flumazenil, which counteracts benzodiazepines and is often used to treat people who overdose on those drugs. After an injection of flumazenil, the patients improved to near-normal levels on several measures of alertness and vigilance, the researchers report. Rye says these effects lasted up to a couple hours.
In hopes of longer-lasting benefits, the researchers persuaded the pharmaceutical company Hoffmann-La Roche, which makes the drug, to donate a powdered form that can be incorporated into dissolvable tablets taken under the tongue and a cream applied to the skin. One 30-something patient has been taking these formulations for 4 years and has improved dramatically, the researchers report in the paper. She has resumed her career as an attorney, from which her hypersomnia had forced her to take a leave of absence.
The findings are “certainly provocative,” Saper says, although they’ll have to be replicated in a larger, double-blind trial to be truly convincing.
Even so, says Phyllis Zee, a neurologist at Northwestern University in Evanston, Illinois: “This gives us a new window into thinking about treatments” for primary hypersomnia. “These patients don’t respond well to stimulants,” Zee says, so a better strategy may be to inhibit the sleep-promoting effects of GABA—or as Rye puts it, releasing the parking brake instead of pressing the accelerator.
The next steps are clear, Rye says: Identify the mystery compound, figure out a faster way to detect it, and conduct a larger clinical trial to test the benefits of flumazenil. However, the researchers first need someone to fund such a study. So far, Rye says, they’ve gotten no takers.
http://news.sciencemag.org/sciencenow/2012/11/putting-themselves-to-sleep.html
Scientists create artifical brain with 2.3 million simulated neurons
Another computer is setting its wits to perform human tasks. But this computer is different. Instead of the tour de force processing of Deep Blue or Watson’s four terabytes of facts of questionable utility, Spaun attempts to play by the same rules as the human brain to figure things out. Instead of the logical elegance of a CPU, Spaun’s computations are performed by 2.3 million simulated neurons configured in networks that resemble some of the brain’s own networks. It was given a series of tasks and performed pretty well, taking a significant step toward the creation of a simulated brain.
Spaun stands for Semantic Pointer Architecture: Unified Network. It was given 6 different tasks that tested its ability to recognize digits, recall from memory, add numbers and complete patterns. Its cognitive network simulated the prefrontal cortex to handle working memory and the basal ganglia and thalamus to control movements. Like a human, Spaun can view an image and then give a motor response; that is, it is presented images that it sees through a camera and then gives a response by drawing with a robotic arm.
And its performance was similar to that of a human brain. For example, the simplest task, image recognition, Spaun was shown various numbers and asked to draw what it sees. It got 94 percent of the numbers correct. In a working memory task, however, it didn’t do as well. It was shown a series of random numbers and then asked to draw them in order. Like us with human brains, Spaun found the pattern recognition task easy, the working memory task not quite as easy.
The important thing here is not how well Spaun performed on the tasks – your average computer could find ways to perform much better than Spaun. But what’s important is that, in Spaun’s case, the task computations were carried out solely by the 2.3 million artificial neurons spiking in the way real neurons spike to carry information from one neuron to another. The visual image, for example, was processed hierarchically, with multiple levels of neurons successively extracting more complex information, just as the brain’s visual system does. Similarly, the motor response mimicked the brain’s strategy of combining many simple movements to produce an optimal, single movement while drawing.
Chris Eliasmith, from the University of Waterlook in Ontario, Canada and lead author of the study is happy with his cognitive creation. “It’s not as smart as monkeys when it comes to categorization,” he told CNN, “but it’s actually smarter than monkeys when it comes to recognizing syntactic patterns, structured patterns in the input, that monkeys won’t recognize.”
Watch Spaun work through its tasks in the following video.
One thing Spaun can’t do is perform tasks in realtime. Every second you saw Spaun performing tasks in the video actually requires 2.5 hours of numbers crunching by its artificial brain. The researchers hope to one day have it perform in realtime.
It’s important to note that Spaun isn’t actually learning anything by performing these tasks. Its neural nets are hardwired and are incapable of the modifications that real neurons undergo when we learn. But producing complex behavior from a simulated neuronal network still represents an important initial step toward building an artificial brain. Christian Machens, a neuroscientist at the Champalimaud Neuroscience Programme in Lisbon and was not involved in the study, writes in Science that the strategy for building a simulated brain is “to not simply incorporate the largest number of neurons or the greatest amount of detail, but to reproduce the largest amount of functionality and behavior.”
We’re still a long way from artificial intelligence that is sentient and self-aware. And there’s no telling if the robots of the future will have brains that look like ours or if entirely different solutions will be used to produce complex behavior. Whatever it looks like, Spaun is a noble step in the right direction.
Scientists Create Artificial Brain With 2.3 Million Simulated Neurons
Diuretic Drug Offers Latest Hope for Autism Treatment
A drug used for decades to treat high blood pressure and other conditions has shown promise in a small clinical trial for autism. The drug, bumetanide, reduced the overall severity of behavioral symptoms after 3 months of daily treatment. The researchers say that many parents of children who received the drug reported that their children were more “present” and engaged in social interactions after taking it. The new findings are among several recent signs that treatments to address the social deficits at the core of autism may be on the horizon.
Several lines of evidence suggest that autism interferes with the neurotransmitter GABA, which typically puts a damper on neural activity. Bumetanide may enhance the inhibitory effects of GABA, and the drug has been used safely as a diuretic to treat a wide range of heart, lung, and kidney conditions. In the new study, researchers led by Yehezkel Ben-Ari at the Mediterranean Institute of Neurobiology in Marseille, France, recruited 60 autistic children between the ages of 3 and 11 and randomly assigned them to receive either a daily pill of bumetanide or a placebo. (Neither the children’s parents nor the researchers who assessed the children knew who received the actual drug.)
As a group, those who got bumetanide improved by 5.6 points on a 60-point scale that’s often used to assess behaviors related to autism, the researchers report today in Translational Psychiatry. That was enough to nudge the group average just under the cutoff for severe autism and into the mild to medium category. The study did not look directly at whether the drug improved all symptoms equally or some more than others. “We have some indications that the symptoms particularly ameliorated with bumetanide are the genuine core symptoms of autism, namely communication and social interactions,” Ben-Ari says. More work will be needed to verify that impression. Ben-Ari says his team is now preparing for a larger, multicenter trial in Europe.
The current study already looks interesting to some. “It’s enough to make me think about trying it in a few of my autism patients who haven’t responded to other interventions,” says Randi Hagerman, a pediatrician who studies neurodevelopmental disorders at the University of California, Davis. Social interactions tend to be reinforcing, Hagerman adds, so getting an autistic child to start interacting more can have a positive effect on subsequent brain development.
Other drugs have recently shown promise for autism. In September, Hagerman and colleagues reported that arbaclofen, a drug that stimulates a type of GABA receptor, reduced social avoidance in people with fragile X syndrome, a genetic disorder that shares many features with autism. Many researchers are also hopeful about clinical trials under way with drugs that block certain receptors for glutamate, the main neurotransmitter in the brain that excites neural activity. Results from those trials should come out next year.
All of this work, including the new study, suggests that drugs that reduce neural excitation by blocking glutamate or enhance inhibition by boosting GABA may be helpful for treating autism, says Elizabeth Berry-Kravis, a pediatric neurologist at Rush University in Chicago, Illinois, and a collaborator on the recent arbaclofen study. “There seems to be this imbalance between excitation and inhibition in people with autism.”
That’s a potentially game-changing insight. Now doctors can only prescribe drugs that treat individual symptoms of autism rather than the underlying cause of the disorder, Berry-Kravis says. Doctors often prescribe antipsychotic drugs to reduce irritability, for example, but those drugs don’t address the social and communication problems at the heart of the disorder. “It’s exciting that now we’re thinking about the underlying mechanisms and treating those.”
http://news.sciencemag.org/sciencenow/2012/12/diuretic-drug-offers-latest-hope.html
Mother-Child Connection: Scientists Discover Children’s Cells Living in Mothers’ Brains, Including Male Cells Living in the Female Brain for Decades
The link between a mother and child is profound, and new research suggests a physical connection even deeper than anyone thought. The profound psychological and physical bonds shared by the mother and her child begin during gestation when the mother is everything for the developing fetus, supplying warmth and sustenance, while her heartbeat provides a soothing constant rhythm.
The physical connection between mother and fetus is provided by the placenta, an organ, built of cells from both the mother and fetus, which serves as a conduit for the exchange of nutrients, gasses, and wastes. Cells may migrate through the placenta between the mother and the fetus, taking up residence in many organs of the body including the lung, thyroid muscle, liver, heart, kidney and skin. These may have a broad range of impacts, from tissue repair and cancer prevention to sparking immune disorders.
It is remarkable that it is so common for cells from one individual to integrate into the tissues of another distinct person. We are accustomed to thinking of ourselves as singular autonomous individuals, and these foreign cells seem to belie that notion, and suggest that most people carry remnants of other individuals. As remarkable as this may be, stunning results from a new study show that cells from other individuals are also found in the brain. In this study, male cells were found in the brains of women and had been living there, in some cases, for several decades. What impact they may have had is now only a guess, but this study revealed that these cells were less common in the brains of women who had Alzheimer’s disease, suggesting they may be related to the health of the brain.
We all consider our bodies to be our own unique being, so the notion that we may harbor cells from other people in our bodies seems strange. Even stranger is the thought that, although we certainly consider our actions and decisions as originating in the activity of our own individual brains, cells from other individuals are living and functioning in that complex structure. However, the mixing of cells from genetically distinct individuals is not at all uncommon. This condition is called chimerism after the fire-breathing Chimera from Greek mythology, a creature that was part serpent part lion and part goat. Naturally occurring chimeras are far less ominous though, and include such creatures as the slime mold and corals.
Microchimerism is the persistent presence of a few genetically distinct cells in an organism. This was first noticed in humans many years ago when cells containing the male “Y” chromosome were found circulating in the blood of women after pregnancy. Since these cells are genetically male, they could not have been the women’s own, but most likely came from their babies during gestation.
In this new study, scientists observed that microchimeric cells are not only found circulating in the blood, they are also embedded in the brain. They examined the brains of deceased women for the presence of cells containing the male “Y” chromosome. They found such cells in more than 60 percent of the brains and in multiple brain regions. Since Alzheimer’s disease is more common in women who have had multiple pregnancies, they suspected that the number of fetal cells would be greater in women with AD compared to those who had no evidence for neurological disease. The results were precisely the opposite: there were fewer fetal-derived cells in women with Alzheimer’s. The reasons are unclear.
Microchimerism most commonly results from the exchange of cells across the placenta during pregnancy, however there is also evidence that cells may be transferred from mother to infant through nursing. In addition to exchange between mother and fetus, there may be exchange of cells between twins in utero, and there is also the possibility that cells from an older sibling residing in the mother may find their way back across the placenta to a younger sibling during the latter’s gestation. Women may have microchimeric cells both from their mother as well as from their own pregnancies, and there is even evidence for competition between cells from grandmother and infant within the mother.
What it is that fetal microchimeric cells do in the mother’s body is unclear, although there are some intriguing possibilities. For example, fetal microchimeric cells are similar to stem cells in that they are able to become a variety of different tissues and may aid in tissue repair. One research group investigating this possibility followed the activity of fetal microchimeric cells in a mother rat after the maternal heart was injured: they discovered that the fetal cells migrated to the maternal heart and differentiated into heart cells helping to repair the damage. In animal studies, microchimeric cells were found in maternal brains where they became nerve cells, suggesting they might be functionally integrated in the brain. It is possible that the same may true of such cells in the human brain.
These microchimeric cells may also influence the immune system. A fetal microchimeric cell from a pregnancy is recognized by the mother’s immune system partly as belonging to the mother, since the fetus is genetically half identical to the mother, but partly foreign, due to the father’s genetic contribution. This may “prime” the immune system to be alert for cells that are similar to the self, but with some genetic differences. Cancer cells which arise due to genetic mutations are just such cells, and there are studies which suggest that microchimeric cells may stimulate the immune system to stem the growth of tumors. Many more microchimeric cells are found in the blood of healthy women compared to those with breast cancer, for example, suggesting that microchimeric cells can somehow prevent tumor formation. In other circumstances, the immune system turns against the self, causing significant damage. Microchimerism is more common in patients suffering from Multiple Sclerosis than in their healthy siblings, suggesting chimeric cells may have a detrimental role in this disease, perhaps by setting off an autoimmune attack.
This is a burgeoning new field of inquiry with tremendous potential for novel findings as well as for practical applications. But it is also a reminder of our interconnectedness.
The Death of “Near Death” Experiences ?
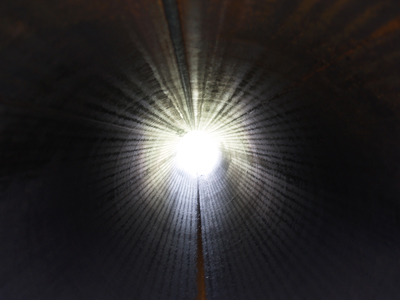
You careen headlong into a blinding light. Around you, phantasms of people and pets lost. Clouds billow and sway, giving way to a gilded and golden entrance. You feel the air, thrusted downward by delicate wings. Everything is soothing, comforting, familiar. Heaven.
It’s a paradise that some experience during an apparent demise. The surprising consistency of heavenly visions during a “near death experience” (or NDE) indicates for many that an afterlife awaits us. Religious believers interpret these similar yet varying accounts like blind men exploring an elephant—they each feel something different (the tail is a snake and the legs are tree trunks, for example); yet all touch the same underlying reality. Skeptics point to the curious tendency for Heaven to conform to human desires, or for Heaven’s fleeting visage to be so dependent on culture or time period.
Heaven, in a theological view, has some kind of entrance. When you die, this entrance is supposed to appear—a Platform 9 ¾ for those running towards the grave. Of course, the purported way to see Heaven without having to take the final run at the platform wall is the NDE. Thrust back into popular consciousness by a surgeon claiming that “Heaven is Real,” the NDE has come under both theological and scientific scrutiny for its supposed ability to preview the great gig in the sky.
But getting to see Heaven is hell—you have to die. Or do you?
This past October, neurosurgeon Dr. Eben Alexander claimed that “Heaven is Real”, making the cover of the now defunct Newsweek magazine. His account of Heaven was based on a series of visions he had while in a coma, suffering the ravages of a particularly vicious case of bacterial meningitis. Alexander claimed that because his neocortex was “inactivated” by this malady, his near death visions indicated an intellect apart from the grey matter, and therefore a part of us survives brain-death.
Alexander’s resplendent descriptions of the afterlife were intriguing and beautiful, but were also promoted as scientific proof. Because Alexander was a brain “scientist” (more accurately, a brain surgeon), his account carried apparent weight.
Scientifically, Alexander’s claims have been roundly criticized. Academic clinical neurologist Steve Novella removes the foundation of Alexander’s whole claim by noting that his assumption of cortex “inactivation” is flawed:
Alexander claims there is no scientific explanation for his experiences, but I just gave one. They occurred while his brain function was either on the way down or on the way back up, or both, not while there was little to no brain activity.
In another takedown of the popular article, neuroscientist Sam Harris (with characteristic sharpness) also points out this faulty premise, and notes that Alexander’s evidence for such inactivation is lacking:
The problem, however, is that “CT scans and neurological examinations” can’t determine neuronal inactivity—in the cortex or anywhere else. And Alexander makes no reference to functional data that might have been acquired by fMRI, PET, or EEG—nor does he seem to realize that only this sort of evidence could support his case.
Without a scientific foundation for Alexander’s claims, skeptics suggest he had a NDE later fleshed out by confirmation bias and colored by culture. Harris concludes in a follow-up post on his blog, “I am quite sure that I’ve never seen a scientist speak in a manner more suggestive of wishful thinking. If self-deception were an Olympic sport, this is how our most gifted athletes would appear when they were in peak condition.”
And these takedowns have company. Paul Raeburn in the Huffington Post, speaking of Alexander’s deathbed vision being promoted as a scientific account, wrote, “We are all demeaned, and our national conversation is demeaned, by people who promote this kind of thing as science. This is religious belief; nothing else.” We might expect this tone from skeptics, but even the faithful chime in. Greg Stier writes in the Christian post that while he fully believes in the existence of Heaven, we should not take NDE accounts like Alexander’s as proof of it.
These criticisms of Alexander point out that what he saw was a classic NDE—the white light, the tunnel, the feelings of connectedness, etc. This is effective in dismantling his account of an “immaterial intellect” because, so far, most symptoms of a NDE are in fact scientifically explainable. [ another article on this site provides a thorough description of the evidence, as does this study.]
One might argue that the scientific description of NDE symptoms is merely the physical account of what happens as you cross over. A brain without oxygen may experience “tunnel vision,” but a brain without oxygen is also near death and approaching the afterlife, for example. This argument rests on the fact that you are indeed dying. But without the theological gymnastics, I think there is an overlooked yet critical aspect to the near death phenomenon, one that can render Platform 9 ¾ wholly solid. Studies have shown that you don’t have to be near death to have a near death experience.
“Dying”
In 1990, a study was published in the Lancet that looked at the medical records of people who experienced NDE-like symptoms as a result of some injury or illness. It showed that out of 58 patients who reported “unusual” experiences associated with NDEs (tunnels, light, being outside one’s own body, etc.), 30 of them were not actually in any danger of dying, although they believed they were [1]. The authors of the study concluded that this finding offered support to the physical basis of NDEs, as well as the “transcendental” basis.
Why would the brain react to death (or even imagined death) in such a way? Well, death is a scary thing. Scientific accounts of the NDE characterize it as the body’s psychological and physiological response mechanism to such fear, producing chemicals in the brain that calm the individual while inducing euphoric sensations to reduce trauma.
Imagine an alpine climber whose pick fails to catch the next icy outcropping as he or she plummets towards a craggy mountainside. If one truly believes the next experience he or she will have is an intimate acquainting with a boulder, similar NDE-like sensations may arise (i.e., “My life flashed before my eyes…”). We know this because these men and women have come back to us, emerging from a cushion of snow after their fall rather than becoming a mountain’s Jackson Pollock installation.
You do not have to be, in reality, dying to have a near-death experience. Even if you are dying (but survive), you probably won’t have one. What does this make of Heaven? It follows that if you aren’t even on your way to the afterlife, the scientifically explicable NDE symptoms point to neurology, not paradise.
This Must Be the Place
Explaining the near death experience in a purely physical way is not to say that people cannot have a transformative vision or intense mental journey. The experience is real and tells us quite a bit about the brain (while raising even more fascinating questions about consciousness). But emotional and experiential gravitas says nothing of Heaven, or the afterlife in general. A healthy imbibing of ketamine can induce the same feelings, but rarely do we consider this euphoric haze a glance of God’s paradise.
In this case, as in science, a theory can be shot through with experimentation. As Richard Feynman said, “It doesn’t matter how beautiful your theory is, it doesn’t matter how smart you are. If it doesn’t agree with experiment, it’s wrong.
The experiment is exploring an NDE under different conditions. Can the same sensations be produced when you are in fact not dying? If so, your rapping on the Pearly Gates is an illusion, even if Heaven were real. St. Peter surely can tell the difference between a dying man and a hallucinating one.
The near death experience as a foreshadowing of Heaven is a beautiful theory perhaps, but wrong.
Barring a capricious conception of “God’s plan,” one can experience a beautiful white light at the end of a tunnel while still having a firm grasp of their mortal coil. This is the death of near death. Combine explainable symptoms with a plausible, physical theory as to why we have them and you get a description of what it is like to die, not what it is like to glimpse God.
Sitting atop clouds fluffy and white, Heaven may be waiting. We can’t prove that it is not. But rather than helping to clarify, the near death experience, not dependent on death, may only point to an ever interesting and complex human brain, nothing more.
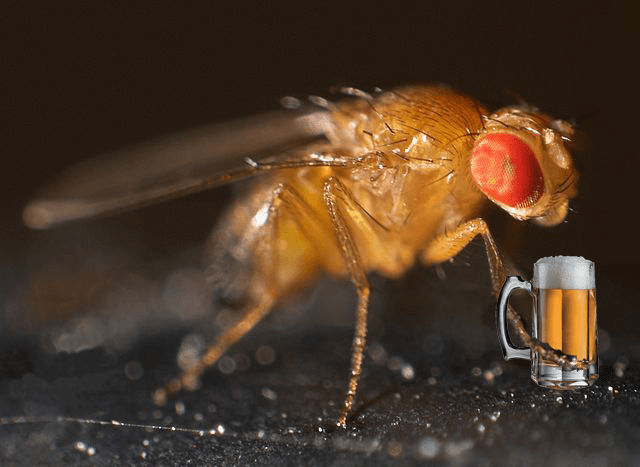
Sexually-deprived fruitflies drink more alcohol
Rejection stinks. It literally hurts. But worse, it has an immediate and negative impact on our brains, producing withdrawal symptoms as if we’re quitting a serious addiction cold turkey. It’s no wonder, then, that we are tempted to turn to drugs to makeourselves feel better. But we’re not the only species that drowns our sorrows when we’re lonely – as a new study in Science reveals, rejected Drosophila do, too. Scientists have found not only will these sexually frustrated flies choose to consume more alcohol than their happily mated peers, sex and alcohol consumption activate the same neurological pathway in their brains.
Drosophila melanogaster males sure know how to woo a lady. When placed in the same container as a potential mate, a male fly will play her a delicate love song by vibrating one wing, caress her rear end, and gently nuzzle her most private of parts with his proboiscis to convince her that he is one heck of a lover. But even the most romantic fly can’t convince an already mated female Drosophila to give up the goods, so scientists were able to use the girls’ steely resolve to see how rejection affects fly drinking behavior.
“Alcohol is one of the most widely used and abused drugs in the world,” explains lead author Galit Shohat-Ophir. “The fruit fly Drosophila melanogaster is an ideal model organism to study how the social environment modulates behavior.” Previous studies have found that Drosophila melanogaster exhibit complex addiction-like behaviors. So in the controlled setting of Ulrike Heberlein’s lab at the University of California San Francisco, researchers paired male fruit flies with three types of females: 1) unmated females, which were willing and happy to mate; 2) mated females, which actively rejected the men; and 3) decapitated females, which didn’t actively reject the guys but, well, weren’t exactly willing partners either. After the flies were satisfied or frustrated, they were offered regular food and food spiked with ethanol, and the researchers measured which type they preferred to see if there was any connection between sex and drinking.
The flies that were rejected drank significantly more than their satisfied peers, but so did the ones paired with incapacitated girls, suggesting that it wasn’t the social aspect of rejection but sexual deprivation that drives male flies to increase their ethanol consumption (see the video at the end!). This alcoholic behavior was very directly related to the guy fly ever getting laid, for even after days of blue balls, if he was allowed to spend some time with a willing woman, he no longer preferred the spiked food.
What the scientists really wanted to understand, though, was why. What drives a frustrated fly to the flask? So to look at the underlying mechanism of this phenomenon, the scientists examined the flies’ brains. A body of scientific literature has connected one particular neurotransmitter, neuropeptide F (NPF), to ethanol-related behaviors in Drosophila, so it was a logical place to start. A very similar neurotransmitter in our brains, called neuropeptide Y (NPY), is linked to alcoholism.
The team found that sexual frustration caused an immediate decrease in the expression of NPF, while sex increased expression. Furthermore, when they used genetics to artificially knock down NPF levels in the satisfied flies, they drank as much as their not-so-satisfied friends. Similarly, when the researchers artificially increased NPF levels, flies stayed sober. This is the first time NPF levels have connected sexual activity to drinking. Clearly, NPF levels controlled the flies’ desire to drink, so the team further explored how NPF works in the fly’s brain.
Many animals, including ourselves, possess a neurological reward system which reinforces good behavior. Through this system, we ascribe pleasure or positive feelings to things we do that are necessary for species survival, including sex, eating, and social interaction. Drugs tap into this system, stimulating pleasure which can lead to addiction. Previous studies have shown that flies find intoxication rewarding, so the researchers hypothesized that NPF may play a role in the reward system.
Preference tests showed that artificially increasing NPF levels in the absence of sex or ethanol was rewarding to the flies, confirming the scientists’ hypothesis. This was further supported by the discovery that constantly activating NPF abolished the flies’ tendency to consider ethanol rewarding.
“NPF is a currency of reward” explains Shohat-Ophir. High NPF levels signal good behavior in Drosophila brains, thus reinforcing any activities which led to that state. This is a truly novel discovery, for while NPF and the mammal version, NPY, have been linked to alcohol consumption, no animal model has ever placed NPF/NPY in the reward system.
Understanding the role of NPF in reward-seeking behaviors may lead to better treatments for addicts. “In mammals, including humans, NPY may have a similar role [as NPF],” says Shohat-Ophir. “If so, one could argue that activating the NPY system in the proper brain regions might reverse the detrimental effects of traumatic and stressful experiences, which often lead to drug abuse.” Already, NPY and drugs that affect the function of its receptors are in clinical trials for anxiety, PTSD, mood disorders and obesity. This study suggests that perhaps they should be tested as treatment for alcoholism, too, as well as other reward-based addictions.
Research: Shohat-Ophir, G, KR Kaun & R Azanchi (2012). Sexual Deprivation Increases Ethanol Intake in Drosophila. Science 335: 1351-1355.
Click http://blogs.scientificamerican.com/science-sushi/2012/03/15/flies-drink-upon-rejection/
to view a sequence of three videos that show a male fly courting and successfully mating with a female fly, another male fly being rejected by a female, and a male choosing to consume an alcohol-infused solution over a non-alcohol solution. Video © Science/AAAS
Musicians’ Brains Synchronize During Duets
The brain waves of two musicians synchronize when they are performing duet, a new study found, suggesting that there’s a neural blueprint for coordinating actions with others.
A team of scientists at the Max Planck Institute for Human Development in Berlin used electrodes to record the brain waves of 16 pairs of guitarists while they played a sequence from “Sonata in G Major” by Christian Gottlieb Scheidler. In each pair, the two musicians played different voices of the piece. One guitarist was responsible for beginning the song and setting the tempo while the other was instructed to follow.
In 60 trials each, the pairs of musicians showed coordinated brain oscillations — or matching rhythms of neural activity — in regions of the brain associated with social cognition and music production, the researchers said.
“When people coordinate their own actions, small networks between brain regions are formed,” study researcher Johanna Sänger said in a statement. “But we also observed similar network properties between the brains of the individual players, especially when mutual coordination is very important; for example at the joint onset of a piece of music.”
Sänger added that the internal synchronization of the lead guitarists’ brain waves was present, and actually stronger, before the duet began.
“This could be a reflection of the leading player’s decision to begin playing at a certain moment in time,” she explained.
Another Max Planck researcher involved in the study, Ulman Lindenberger, led a similar set of experiments in 2009. But in that study, which was published in the journal BMC Neuroscience, the pairs of guitarists played a song in unison, rather than a duet. Lindenberger and his team at the time observed the same type of coordinated brain oscillations, but noted that the synchronization could have been the result of the similarities of the actions performed by the pairs of musicians.
As the new study involved guitarists who were performing different parts of a song, the researchers say their results provide stronger evidence that there is a neural basis for interpersonal coordination. The team believes people’s brain waves might also synchronize during other types of actions, such as during sports games.
The study was published online![]() Nov. 29 in the journal Frontiers in Human Neuroscience.
Nov. 29 in the journal Frontiers in Human Neuroscience.
http://www.livescience.com/25117-musicians-brains-sync-up-during-duet.html