It’s a paradise that some experience during an apparent demise. The surprising consistency of heavenly visions during a “near death experience” (or NDE) indicates for many that an afterlife awaits us. Religious believers interpret these similar yet varying accounts like blind men exploring an elephant—they each feel something different (the tail is a snake and the legs are tree trunks, for example); yet all touch the same underlying reality. Skeptics point to the curious tendency for Heaven to conform to human desires, or for Heaven’s fleeting visage to be so dependent on culture or time period.
Heaven, in a theological view, has some kind of entrance. When you die, this entrance is supposed to appear—a Platform 9 ¾ for those running towards the grave. Of course, the purported way to see Heaven without having to take the final run at the platform wall is the NDE. Thrust back into popular consciousness by a surgeon claiming that “Heaven is Real,” the NDE has come under both theological and scientific scrutiny for its supposed ability to preview the great gig in the sky.
But getting to see Heaven is hell—you have to die. Or do you?
This past October, neurosurgeon Dr. Eben Alexander claimed that “Heaven is Real”, making the cover of the now defunct Newsweek magazine. His account of Heaven was based on a series of visions he had while in a coma, suffering the ravages of a particularly vicious case of bacterial meningitis. Alexander claimed that because his neocortex was “inactivated” by this malady, his near death visions indicated an intellect apart from the grey matter, and therefore a part of us survives brain-death.
Alexander’s resplendent descriptions of the afterlife were intriguing and beautiful, but were also promoted as scientific proof. Because Alexander was a brain “scientist” (more accurately, a brain surgeon), his account carried apparent weight.
Scientifically, Alexander’s claims have been roundly criticized. Academic clinical neurologist Steve Novella removes the foundation of Alexander’s whole claim by noting that his assumption of cortex “inactivation” is flawed:
Alexander claims there is no scientific explanation for his experiences, but I just gave one. They occurred while his brain function was either on the way down or on the way back up, or both, not while there was little to no brain activity.
In another takedown of the popular article, neuroscientist Sam Harris (with characteristic sharpness) also points out this faulty premise, and notes that Alexander’s evidence for such inactivation is lacking:
The problem, however, is that “CT scans and neurological examinations” can’t determine neuronal inactivity—in the cortex or anywhere else. And Alexander makes no reference to functional data that might have been acquired by fMRI, PET, or EEG—nor does he seem to realize that only this sort of evidence could support his case.
Without a scientific foundation for Alexander’s claims, skeptics suggest he had a NDE later fleshed out by confirmation bias and colored by culture. Harris concludes in a follow-up post on his blog, “I am quite sure that I’ve never seen a scientist speak in a manner more suggestive of wishful thinking. If self-deception were an Olympic sport, this is how our most gifted athletes would appear when they were in peak condition.”
And these takedowns have company. Paul Raeburn in the Huffington Post, speaking of Alexander’s deathbed vision being promoted as a scientific account, wrote, “We are all demeaned, and our national conversation is demeaned, by people who promote this kind of thing as science. This is religious belief; nothing else.” We might expect this tone from skeptics, but even the faithful chime in. Greg Stier writes in the Christian post that while he fully believes in the existence of Heaven, we should not take NDE accounts like Alexander’s as proof of it.
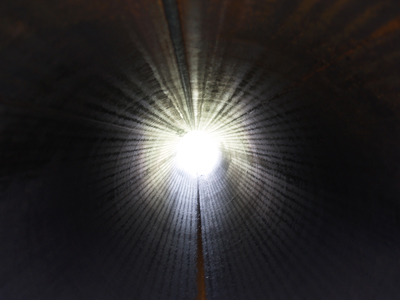
These criticisms of Alexander point out that what he saw was a classic NDE—the white light, the tunnel, the feelings of connectedness, etc. This is effective in dismantling his account of an “immaterial intellect” because, so far, most symptoms of a NDE are in fact scientifically explainable. [ another article on this site provides a thorough description of the evidence, as does this study.]
One might argue that the scientific description of NDE symptoms is merely the physical account of what happens as you cross over. A brain without oxygen may experience “tunnel vision,” but a brain without oxygen is also near death and approaching the afterlife, for example. This argument rests on the fact that you are indeed dying. But without the theological gymnastics, I think there is an overlooked yet critical aspect to the near death phenomenon, one that can render Platform 9 ¾ wholly solid. Studies have shown that you don’t have to be near death to have a near death experience.
“Dying”
In 1990, a study was published in the Lancet that looked at the medical records of people who experienced NDE-like symptoms as a result of some injury or illness. It showed that out of 58 patients who reported “unusual” experiences associated with NDEs (tunnels, light, being outside one’s own body, etc.), 30 of them were not actually in any danger of dying, although they believed they were [1]. The authors of the study concluded that this finding offered support to the physical basis of NDEs, as well as the “transcendental” basis.
Why would the brain react to death (or even imagined death) in such a way? Well, death is a scary thing. Scientific accounts of the NDE characterize it as the body’s psychological and physiological response mechanism to such fear, producing chemicals in the brain that calm the individual while inducing euphoric sensations to reduce trauma.
Imagine an alpine climber whose pick fails to catch the next icy outcropping as he or she plummets towards a craggy mountainside. If one truly believes the next experience he or she will have is an intimate acquainting with a boulder, similar NDE-like sensations may arise (i.e., “My life flashed before my eyes…”). We know this because these men and women have come back to us, emerging from a cushion of snow after their fall rather than becoming a mountain’s Jackson Pollock installation.
You do not have to be, in reality, dying to have a near-death experience. Even if you are dying (but survive), you probably won’t have one. What does this make of Heaven? It follows that if you aren’t even on your way to the afterlife, the scientifically explicable NDE symptoms point to neurology, not paradise.
This Must Be the Place
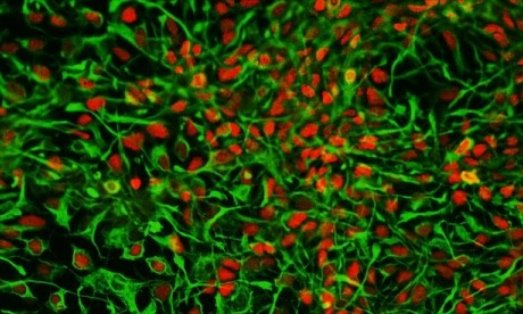
Explaining the near death experience in a purely physical way is not to say that people cannot have a transformative vision or intense mental journey. The experience is real and tells us quite a bit about the brain (while raising even more fascinating questions about consciousness). But emotional and experiential gravitas says nothing of Heaven, or the afterlife in general. A healthy imbibing of ketamine can induce the same feelings, but rarely do we consider this euphoric haze a glance of God’s paradise.
In this case, as in science, a theory can be shot through with experimentation. As Richard Feynman said, “It doesn’t matter how beautiful your theory is, it doesn’t matter how smart you are. If it doesn’t agree with experiment, it’s wrong.
The experiment is exploring an NDE under different conditions. Can the same sensations be produced when you are in fact not dying? If so, your rapping on the Pearly Gates is an illusion, even if Heaven were real. St. Peter surely can tell the difference between a dying man and a hallucinating one.
The near death experience as a foreshadowing of Heaven is a beautiful theory perhaps, but wrong.
Barring a capricious conception of “God’s plan,” one can experience a beautiful white light at the end of a tunnel while still having a firm grasp of their mortal coil. This is the death of near death. Combine explainable symptoms with a plausible, physical theory as to why we have them and you get a description of what it is like to die, not what it is like to glimpse God.
Sitting atop clouds fluffy and white, Heaven may be waiting. We can’t prove that it is not. But rather than helping to clarify, the near death experience, not dependent on death, may only point to an ever interesting and complex human brain, nothing more.
http://blogs.scientificamerican.com/guest-blog/2012/12/03/the-death-of-near-death-even-if-heaven-is-real-you-arent-seeing-it/