There are a few things we take for granted in social interactions with people. We presume that we see the world in roughly the same way, that we all know certain basic facts, that words mean the same things to you as they do to me. And we assume that we have pretty similar ideas of right and wrong.
But for a small – but not that small – subset of the population, things are very different. These people lack remorse and empathy and feel emotion only shallowly. In extreme cases, they might not care whether you live or die. These people are called psychopaths. Some of them are violent criminals, murderers. But by no means all.
Professor Robert Hare is a criminal psychologist, and the creator of the PCL-R, a psychological assessment used to determine whether someone is a psychopath. For decades, he has studied people with psychopathy, and worked with them, in prisons and elsewhere. “It stuns me, as much as it did when I started 40 years ago, that it is possible to have people who are so emotionally disconnected that they can function as if other people are objects to be manipulated and destroyed without any concern,” he says.
Our understanding of the brain is still in its infancy, and it’s not so many decades since psychological disorders were seen as character failings. Slowly we are learning to think of mental illnesses as illnesses, like kidney disease or liver failure, and developmental disorders, such as autism, in a similar way. Psychopathy challenges this view. “A high-scoring psychopath views the world in a very different way,” says Hare. “It’s like colour-blind people trying to understand the colour red, but in this case ‘red’ is other people’s emotions.”
At heart, Hare’s test is simple: a list of 20 criteria, each given a score of 0 (if it doesn’t apply to the person), 1 (if it partially applies) or 2 (if it fully applies). The list in full is: glibness and superficial charm, grandiose sense of self-worth, pathological lying, cunning/manipulative, lack of remorse, emotional shallowness, callousness and lack of empathy, unwillingness to accept responsibility for actions, a tendency to boredom, a parasitic lifestyle, a lack of realistic long-term goals, impulsivity, irresponsibility, lack of behavioural control, behavioural problems in early life, juvenile delinquency, criminal versatility, a history of “revocation of conditional release” (ie broken parole), multiple marriages, and promiscuous sexual behaviour. A pure, prototypical psychopath would score 40. A score of 30 or more qualifies for a diagnosis of psychopathy. Hare says: “A friend of mine, a psychiatrist, once said: ‘Bob, when I meet someone who scores 35 or 36, I know these people really are different.’ The ones we consider to be alien are the ones at the upper end.”
But is psychopathy a disorder – or a different way of being? Anyone reading the list above will spot a few criteria familiar from people they know. On average, someone with no criminal convictions scores 5. “It’s dimensional,” says Hare. “There are people who are part-way up the scale, high enough to warrant an assessment for psychopathy, but not high enough up to cause problems. Often they’re our friends, they’re fun to be around. They might take advantage of us now and then, but usually it’s subtle and they’re able to talk their way around it.” Like autism, a condition which we think of as a spectrum, “psychopathy”, the diagnosis, bleeds into normalcy.
We think of psychopaths as killers, criminals, outside society. People such as Joanna Dennehy, a 31-year-old British woman who killed three men in 2013 and who the year before had been diagnosed with a psychopathic personality disorder, or Ted Bundy, the American serial killer who is believed to have murdered at least 30 people and who said of himself: “I’m the most cold-blooded son of a bitch you’ll ever meet. I just liked to kill.” But many psychopathic traits aren’t necessarily disadvantages – and might, in certain circumstances, be an advantage. For their co-authored book, “Snakes in suits: When Psychopaths go to work”, Hare and another researcher, Paul Babiak, looked at 203 corporate professionals and found about four per cent scored sufficiently highly on the PCL-R to be evaluated for psychopathy. Hare says that this wasn’t a proper random sample (claims that “10 per cent of financial executives” are psychopaths are certainly false) but it’s easy to see how a lack of moral scruples and indifference to other people’s suffering could be beneficial if you want to get ahead in business.
“There are two kinds of empathy,” says James Fallon, a neuroscientist at the University of California and author of The Psychopath Inside: A Neuroscientist’s Personal Journey into the Dark Side of the Brain. “Cognitive empathy is the ability to know what other people are feeling, and emotional empathy is the kind where you feel what they’re feeling.” Autistic people can be very empathetic – they feel other people’s pain – but are less able to recognise the cues we read easily, the smiles and frowns that tell us what someone is thinking. Psychopaths are often the opposite: they know what you’re feeling, but don’t feel it themselves. “This all gives certain psychopaths a great advantage, because they can understand what you’re thinking, it’s just that they don’t care, so they can use you against yourself.” (Chillingly, psychopaths are particularly adept at detecting vulnerability. A 2008 study that asked participants to remember virtual characters found that those who scored highly for psychopathy had a near perfect recognition for sad, unsuccessful females, but impaired memory for other characters.)
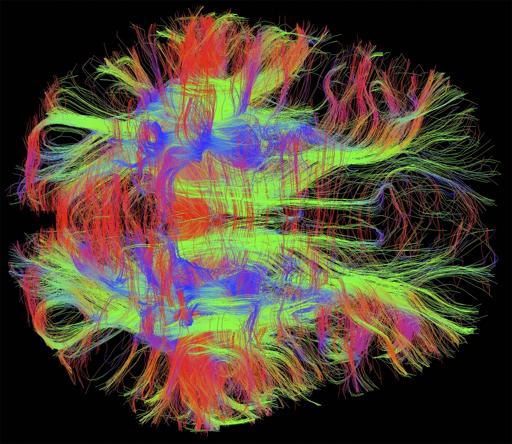
Fallon himself is a case in point. In 2005, he was looking at brain scans of psychopathic murderers, while on another study, of Alzheimer’s, he was using scans of his own family’s brains as controls. In the latter pile, he found something strange. “You can’t tell just from a brain scan whether someone’s a psychopath,” he says, “but you can make a good guess at the personality traits they’ll have.” He describes a great loop that starts in the front of the brain including the parahippocampal gyrus and the amygdala and other regions tied to emotion and impulse control and empathy. Under certain circumstances they would light up dramatically on a normal person’s MRI scan, but would be darker on a psychopath’s.
“I saw one that was extremely abnormal, and I thought this is someone who’s way off. It looked like the murderers I’d been looking at,” he says. He broke the anonymisation code in case it had been put into the wrong pile. When he did, he discovered it was his own brain. “I kind of blew it off,” he says. “But later, some psychiatrist friends of mine went through my behaviours, and they said, actually, you’re probably a borderline psychopath.”
Speaking to him is a strange experience; he barely draws breath in an hour, in which I ask perhaps three questions. He explains how he has frequently put his family in danger, exposing his brother to the deadly Marburg virus and taking his son trout-fishing in the African countryside knowing there were lions around. And in his youth, “if I was confronted by authority – if I stole a car, made pipe bombs, started fires – when we got caught by the police I showed no emotion, no anxiety”. Yet he is highly successful, driven to win. He tells me things most people would be uncomfortable saying: that his wife says she’s married to a “fun-loving, happy-go-lucky nice guy” on the one hand, and a “very dark character who she does not like” on the other. He’s pleasant, and funny, if self-absorbed, but I can’t help but think about the criteria in Hare’s PCL-R: superficial charm, lack of emotional depth, grandiose sense of self-worth. “I look like hell now, Tom,” he says – he’s 66 – “but growing up I was good-looking, six foot, 180lb, athletic, smart, funny, popular.” (Hare warns against non-professionals trying to diagnose people using his test, by the way.)
“Psychopaths do think they’re more rational than other people, that this isn’t a deficit,” says Hare. “I met one offender who was certainly a psychopath who said ‘My problem is that according to psychiatrists I think more with my head than my heart. What am I supposed to do about that? Am I supposed to get all teary-eyed?’ ” Another, asked if he had any regrets about stabbing a robbery victim, replied: “Get real! He spends a few months in hospital and I rot here. If I wanted to kill him I would have slit his throat. That’s the kind of guy I am; I gave him a break.”
And yet, as Hare points out, when you’re talking about people who aren’t criminals, who might be successful in life, it’s difficult to categorise it as a disorder. “It’d be pretty hard for me to go into high-level political or economic or academic context and pick out all the most successful people and say, ‘Look, I think you’ve got some brain deficit.’ One of my inmates said that his problem was that he’s a cat in a world of mice. If you compare the brainwave activity of a cat and a mouse, you’d find they were quite different.”
It would, says Hare, probably have been an evolutionarily successful strategy for many of our ancestors, and can be successful today; adept at manipulating people, a psychopath can enter a community, “like a church or a cultural organisation, saying, ‘I believe the same things you do’, but of course what we have is really a cat pretending to be a mouse, and suddenly all the money’s gone”. At this point he floats the name Bernie Madoff.
This brings up the issue of treatment. “Psychopathy is probably the most pleasant-feeling of all the mental disorders,” says the journalist Jon Ronson, whose book, The Psychopath Test, explored the concept of psychopathy and the mental health industry in general. “All of the things that keep you good, morally good, are painful things: guilt, remorse, empathy.” Fallon agrees: “Psychopaths can work very quickly, and can have an apparent IQ higher than it really is, because they’re not inhibited by moral concerns.”
So psychopaths often welcome their condition, and “treating” them becomes complicated. “How many psychopaths go to a psychiatrist for mental distress, unless they’re in prison? It doesn’t happen,” says Hare. The ones in prison, of course, are often required to go to “talk therapy, empathy training, or talk to the family of the victims” – but since psychopaths don’t have any empathy, it doesn’t work. “What you want to do is say, ‘Look, it’s in your own self-interest to change your behaviour, otherwise you’ll stay in prison for quite a while.’ ”
It seems Hare’s message has got through to the UK Department of Justice: in its guidelines for working with personality-disordered inmates, it advises that while “highly psychopathic individuals” are likely to be “highly treatment resistant”, the “interventions most likely to be effective are those which focus on ‘self-interest’ – what the offender wants out of life – and work with them to develop the skills to get those things in a pro-social rather than anti-social way.”
If someone’s brain lacks the moral niceties the rest of us take for granted, they obviously can’t do anything about that, any more than a colour-blind person can start seeing colour. So where does this leave the concept of moral responsibility? “The legal system traditionally asserts that all people standing in front of the judge’s bench are equal. That’s demonstrably false,” says the neuroscientist David Eagleman, author of Incognito: The Secret Lives of the Brain. He suggests that instead of thinking in terms of blameworthiness, the law should deal with the likelihood that someone will reoffend, and issue sentences accordingly, with rehabilitation for those likely to benefit and long sentences for those likely to be long-term dangers. The PCL-R is already used as part of algorithms which categorise people in terms of their recidivism risk. “Life insurance companies do exactly this sort of thing, in actuarial tables, where they ask: ‘What age do we think he’s going to die?’ No one’s pretending they know exactly when we’re going to die. But they can make rough guesses which make for an enormously more efficient system.”
What this doesn’t mean, he says, is a situation like the sci-fi film Minority Report, in which people who are likely to commit crimes are locked up before they actually do. “Here’s why,” he says. “It’s because many people in the population have high levels of psychopathy – about 1 per cent. But not all of them become criminals. In fact many of them, because of their glibness and charm and willingness to ride roughshod over the people in their way, become quite successful. They become CEOs, professional athletes, soldiers. These people are revered for their courage and their straight talk and their willingness to crush obstacles in their way. Merely having psychopathy doesn’t tell us that a person will go off and commit a crime.” It is central to the justice system, both in Britain and America, that you can’t pre-emptively punish someone. And that won’t ever change, says Eagleman, not just for moral, philosophical reasons, but for practical ones. The Minority Report scenario is a fantasy, because “it’s impossible to predict what somebody will do, even given their personality type and everything, because life is complicated and crime is conceptual. Once someone has committed a crime, once someone has stepped over a societal boundary, then there’s a lot more statistical power about what they’re likely to do in future. But until that’s happened, you can’t ever know.”
Speaking to all these experts, I notice they all talk about psychopaths as “them”, almost as a different species, although they make conscious efforts not to. There’s something uniquely troubling about a person who lacks emotion and empathy; it’s the stuff of changeling stories, the Midwich Cuckoos, Hannibal Lecter. “You know kids who use a magnifying glass to burn ants, thinking, this is interesting,” says Hare. “Translate that to an adult psychopath who treats a person that way. It is chilling.” At one stage Ronson suggests I speak to another well-known self-described psychopath, a woman, but I can’t bring myself to. I find the idea unsettling, as if he’d suggested I commune with the dead.
http://www.telegraph.co.uk/culture/books/10737827/Psychopaths-how-can-you-spot-one.html
Thanks to Steven Weihing for bringing this to the attention of the It’s Interesting community.