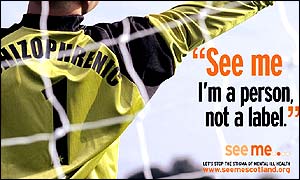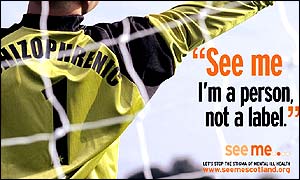

Academia is calling for the abolishment of the term “schizophrenia” in hopes of finding a label that’s less stigmatized. Why people with the medical condition have mixed opinions.
In an article recently published in the academic journal Schizophrenia Research, researchers called for the abolition of the term “schizophrenia.” Renaming the disorder, they argue, could destigmatize the disorder, create greater willingness of people with schizophrenia to pursue treatments, make it easier for doctors to give a diagnosis, and communicate that the prognosis is much less bleak than most people believe.
“Over the last years the term ‘schizophrenia’ has been increasingly contested by patients, families, researchers, and clinicians,” wrote Antonio Lasalvia in an email to The Daily Beast. Lasalvia is one of the study authors and a professor of psychiatry at University of Verona.
“The literature, from both Eastern and Western countries, consistently shows that the term schizophrenia holds a negative stigmatizing connotation. This negative connotation is a barrier for the recognition of the problem itself, for seeking specialized care, for taking full advantage of specialized care. It is therefore useless and sometimes damaging.”
The word “schizophrenia” was coined in the early 20th century, deriving from the Greek word for “split mind.” The term conveyed the idea that people with schizophrenia experienced a splitting of their personality—that they no longer had unified identities.
Considering all the words for mental illness, both those used by medical doctors and those that are cruel slurs used by the general public, it is striking how many of them have connotations of being broken or disorganized: deranged, crazy (which means cracked— itself a derogatory term), unglued, having a screw loose, unhinged, off the wall.
It seems there is some stigma attached to “schizophrenia.” One study showed that most people with schizophrenia (the preferred term is no longer “patients” but “users” or “consumers”) worry that they are viewed unfavorably by others, while some avoid telling people their diagnosis.
Another study examined the use of “schizophrenia” in the news media. Frequently, it is used not to describe a mental disorder, but as a metaphor for inconsistency, or being of a split mind. For example, The Washington Post included an opinion piece that mentioned, “the schizophrenia of a public that wants less government spending, more government services and lower taxes.” It is still socially acceptable—even among many card-carrying progressives—to say that something or someone is “insane,” “crazy,” or “unhinged.”
Christina Bruni, author of Left of the Dial: A Memoir of Schizophrenia, Recovery, and Hope, told me that her experience of stigma has changed over the years. “I used to not want to have ‘schizophrenia’ because I didn’t want people to think I was crazy. After a failed drug holiday, and a failed career in the gray flannel insurance field, I now have a creative job as a librarian,” she wrote in an email. “Ever since I started work as a librarian, I haven’t experienced any stigma in my ordinary life. It’s the people who fall through the cracks, who don’t get help, that the media chronicles, thus reinforcing stereotypes.”
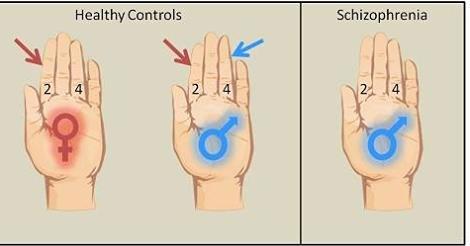
Several people I spoke to noted that the general public confuses schizophrenia with dissociative identity disorder (which used to be known as multiple personality disorder), perhaps because they associate the word schizophrenia with “splitting.” The name change might make the distinction clearer.
There has been precedence for such a move. In addition to dissociative identity disorder, other mental and learning disorders have switched names. For example, “manic-depression” is now widely known as “bipolar disorder,” “mental retardation” is now known as “intellectual and developmental disability.”
“Changing the name can be very successful. What you call something is very important, which is why there is a PR industry,” David Kingdon, professor of psychiatry at the University of Southampton, told The Daily Beast. He has long advocated a change of name for schizophrenia.
Ken Duckworth is the medical director for the National Alliance on Mental Illness. He agrees that a name change has the potential to be powerful, but thinks we need more evidence that it will be effective. “Schizophrenia involves thought, mood, cognition,” he said in an interview. “This is powerful in terms of your identity. It’s not the same as saying you have diabetes. It comes across as something that’s wrong, something that’s negative.”
Kingdon prefers using terms that refer to different forms of psychosis, such as “traumatic psychosis” and “drug-induced psychosis.” “Clients don’t get so excited about it. It gives insight into treatment,” he says. “You can say, ‘Something can be done about this and what can be done is this.’”
Kingdon emphasized that many people feel hopeless upon receiving a diagnosis of schizophrenia when in fact treatments have improved prognoses dramatically in the last 20 years. “Cognitive behavioral therapy, complementary to medical treatment, has been pretty well-demonstrated to be effective,” he pointed out.
In cognitive behavioral therapy, users learn to recognize when they are having disruptive thoughts and are taught techniques for managing them. A recent study which Kingdon co-authored showed that cognitive behavioral therapy reduced both worry and persecutory delusions. “We don’t hear a lot of media stories of people getting better, but they do all the time,” added Duckworth.
Japan has changed the name of schizophrenia. In 2002, it was recommended that seishin-bunretsu-byo (“mind-split-disease”) become togo-shitcho-sho (“integration dysregulation syndrome”). The change was officially adopted by the Japanese Ministry of Health and Welfare by 2005.
Following the change, doctors in Japan became far more likely to disclose to patients that they had schizophrenia. While this shift occurred during a time in which Japanese doctors in general were becoming more willing to deliver difficult diagnoses to patients, it happened at a much more rapid pace with schizophrenia. This suggests that the name change itself increased doctors’ willingness to talk to their patients.
A large majority of Japanese psychiatrists felt, after the name change, better able to communicate information to patients about the disorder, and also that patients were more likely to adhere to treatment plans.
“The first lesson from the Japanese experience is that a change is possible and that the change may be beneficial for mental health users and their careers, for professionals and researchers alike,” said Lasalvia. “An early effect of renaming schizophrenia, as proven by the Japanese findings, would increase the percentage of patients informed about their diagnosis, prognosis, and available interventions. A name change would facilitate help seeking and service uptake by patients, and would be most beneficial for the provision of psychosocial interventions, since better informed patients generally display a more positive attitude towards care and a more active involvement in their own care programs.”
“It’s an empirical question whether it reduces stigma, and we don’t really know the answer yet,” said John Kane, chairman of psychiatry at the Zucker Hillside Hospital in New York. “The data from Japan certainly support the value of doing it. Given that, it is something that should be considered.”
The U.S. and other Western countries, however, are different from Japan in significant ways. In 1999, only 7 percent of clinicians informed patients of their diagnosis (about a third told families but not the patients).
Doctors in the West do tend to be more open with diagnoses in general. In the case of schizophrenia, however, fewer are. One study of Australian clinicians found that while more than half thought one should deliver a diagnosis of schizophrenia, doctors find reasons in practice to delay or avoid doing so. Some wanted to make absolutely sure the diagnosis was 100 percent correct since it was so potentially devastating. Others were concerned about the patient losing hope—many had a patient commit suicide.
While doctors are reluctant to give diagnoses, caregivers are eager to receive them. One study showed that caregivers unanimously preferred a full diagnosis as soon as possible, and their pain was greatly increased by the fact that their doctors—frequently—avoided talking to them about it. It also seems likely that a disorder’s stigmatization can only increase if even one’s doctor is secretive about it or avoids discussing it.
Tomer Levin is a psychiatrist at Memorial Sloan Kettering Cancer Center who studies doctor-patient communication. He first proposed a name change to schizophrenia almost 10 years ago. “Before the 1980s, ‘cancer’ was a stigmatizing term. The same thing was going on with ‘schizophrenia.’ A stigmatizing term doesn’t help the conversation,” he told The Daily Beast. “Our research is figuring out how to train doctors how to communicate. Say your son or daughter has psychotic break, you’re coping with that. Then you get a diagnosis. It should reflect its neurological roots and be a diagnosis that offers hope.”
Levin suggested Neuro-Emotional Integration Disorder to emphasize both its neural basis and its emotional one. He suggested that while clinicians are often focused on symptoms such as delusions, users are focused on how they feel emotionally: withdrawn, alienated, and isolated.
“We want a term that reflects that this is not just one disorder, but includes many different subtypes. A name should de-catastrophize the worst-case scenario so people don’t panic. We could improve people’s desire to access treatment and family support,” Levin continued. “Cognitive behavioral therapy can be very useful to come to terms with it. With a different name, we can link people into psychotherapy by discussing what illness is, hook them into medication by emphasizing its biological basis.”
A change is also already underway in the UK, with more doctors and patients referring to “psychosis” than “schizophrenia.” Kingdon noted that one competitive scholarship was more successful after its name was changed from National Schizophrenia Fellowship to Rethink. Proposed name changes include Kraepelin–Bleuler Disease (after two of the people who first described and delineated schizophrenia), Neuro-Emotional Integration Disorder, Youth onset CONative, COgnitive and Reality Distortion syndrome (CONCORD), or psychosis.
It is startling to read studies on proposed name changes and realize how few studies have canvassed what people with schizophrenia actually think. But the feelings experiences and feelings of users ought to be decisive. It is they who have actually experienced receiving a diagnosis, telling friends and family, informing other health care practitioners.
Elyn Saks is a law professor at the University of Southern California who specializes in mental health law and is a MacArthur Foundation Fellowship winner. She has written about her experience of schizophrenia in a memoir called The Center Cannot Hold. “We need to consult consumer/patients and see what’s least stigmatizing,” she pointed out. “We’re not a group with a big movement which can speak for us. Consumers should be surveyed.”
Duckworth was on the same page as Saks. “The name change should be driven by people with the illnesses saying, ‘We think we need this,’” he said.
“Schizophrenia is a medical condition. The term doesn’t need to be changed. If the term schizophrenia spooks a person living with the illness, they need to examine why they’re upset,” said Bruni. “The only power the diagnosis has over you is the power you give it. You need to have the balls or breasts to say, ‘OK, I have this condition and it’s something I have. That’s all it is.’ The term ‘schizophrenia’ is in my view a valid reference for what’s going on with the illness: Your thoughts and feelings are in a noisy brawl and there’s no calm unity or peace of mind.”
Kane, too, worries that changing the name might be a matter of semantics. “We might ignore underlying factors contribute to the stigmatization. What’s frightening about schizophrenia is our misperceptions and our lack of knowledge. Changing the name is only one dimension.”
Bruni prefers “schizophrenia” to “psychosis,” since “the word psychosis has been co-opted by people who are proud to be psychotic and not take medication. They think psychosis is a normal life experience.”
“The term psychosis to me conveys a terrifying hell. I doubt using the term psychotic to describe yourself is going to help you succeed in life,” she continued. “Employers don’t want to hire individuals who are actively psychotic.”
On the other hand, Lasalvia pointed out, “Any term might be problematic to someone for some reason. However, the most conservative option would be the use of an eponym, since eponyms are neutral and avoid connotations.”
Saks tended to agree with Lasalvia. “A more benign name can be good in terms of people accepting that they have it,” she said. “Kraepelin-Bleuler Disease might be the way to go, on the model of Down syndrome or Alzheimer’s disease. I’d also like to see it called a ‘spectrum disorder’ to emphasize differences in outcome.”
“With the right treatment, therapy, and support, a person living with schizophrenia can have a full and robust life,” said Bruni. “If you’re actively engaged in doing the things that give you joy, the diagnosis will become irrelevant. My take on this is: ‘Schizophrenia? Ha! I won’t let it defeat me.’ And it hasn’t.”
http://www.thedailybeast.com/articles/2015/03/26/stigmatized-schizophrenia-gets-a-rebrand.html