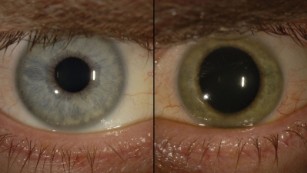
Emerging research suggests pupil dilation in children of depressed mothers when seeing an emotional image can help predict his or her risk of depression over the next two years.
Dr. Brandon Gibb, a professor of psychology at Binghamton University in New York, said the new findings suggest physiological reactivity to sad stimuli can be a potential biomarker of depression risk for some kids.
An important aspect of this finding is that pupillometry is an inexpensive tool that could be administered in family practice or pediatricians’ offices.
The simple test can help identify which children of depressed mothers are at highest risk for developing depression themselves.
“We think this line of research could eventually lead to universal screenings in pediatricians’ offices to assess future depression risk in kids,” said Gibb.
Gibb recruited children whose mothers had a history of major depressive disorder and measured their pupil dilation as they viewed angry, happy, and sad faces.
Follow-up assessments occurred over the next two years, during which structured interviews were used to assess for the children’s level of depressive symptoms, as well as the onset of depressive diagnoses.
Researchers found that a child’s reaction to faces can help predict the risk of developing short-term depression.
Specifically, children exhibiting relatively greater pupil dilation to sad faces experienced higher levels of depressive symptoms during the follow-up period. They also displayed a shorter time to the onset of a clinically significant depressive episode.
Interestingly, the type of emotions displayed by faces were a significant predictor of future depression. That is, the findings were specific to children’s pupil responses to sad faces and were not observed for children’s pupillary reactivity to angry or happy faces.
http://psychcentral.com/news/2015/07/09/new-predictive-test-for-childhood-depression/86632.html