The same bacterium responsible for most stomach ulcers may play a role in the development of Type 2 diabetes among overweight and obese adults, New York University researchers recently reported.
And in the same way that antibiotics eradicate the bacterium and heal ulcers, antibiotics might eventually prove useful in diabetes prevention, they suggest in an article appearing in the Journal of Infectious Diseases.
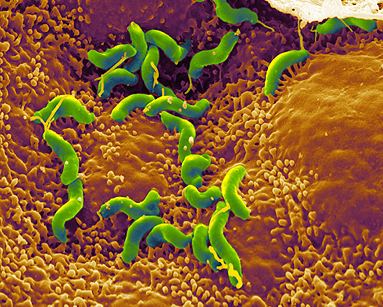
Non-diabetic adults infected with Helicobacter pylori (whether or not they had ulcer symptoms), tended to have higher blood sugar than adults without H. pylori, according to the study co-authored by Yu Chen, an associate professor of environmental medicine at NYU, and Dr. Martin J. Blaser, chairman of NYU’s department of medicine.
Chen and Blaser assessed blood sugar levels using measurements of glycosylated hemoglobin (HbA1c or A1c), a marker of excess glucose in the bloodstream that in recent years has become a key tool for diagnosing and monitoring diabetes.
Helicobacteri pylori is a complicated bacterium. Persistent H. pylori infections beginning in childhood have been linked decades later to ulcers of the stomach and small intestine, and a heightened risk of stomach cancer. Although H. pylori can inflame the stomach, many infected people have no symptoms.
Blaser called H. pylori a complicated and interesting organism that affects children and adults in entirely different ways. In previous work he and Chen found that H. pylori protects children against asthma and allergy.
“This study provides further evidence of late-in-life cost to having H. pylori,” Blaser said in an interview. The findings also give new support to “the concept of eradicating H. pylori in older people.”
Theoretically, antibiotics that wipe out H. pylori might protect older, overweight men and women from developing diabetes, Blaser and Chen said. However, scientists still need to determine how eliminating H. pylori might affect Type 2 diabetes, and how H. pylori affects sugar breakdown among people of different weights.
Chen and Blaser proposed a mechanism for how H. pylori might set the stage for diabetes. They said the bacterium might alter levels of two important digestive hormones, ghrelin and leptin. Ghrelin, sometimes called the hunger hormone, decreases calorie-burning and promotes weight gain. Leptin reduces appetite and boosts calorie-burning. Previous research has linked H. pylori with decreased ghrelin and increased leptin.
In the past, scientists working with small samples came up with conflicting findings about an association between H. pylori and Type 2 diabetes, a chronic disease strongly associated with excess body weight, as well as heredity. Formerly called adult onset or late onset diabetes, Type 2 diabetes has become epidemic among overweight and obese youngsters. It kills an estimated 3.8 million adults worldwide each year.
One of the strengths of the NYU study is that Blaser and Chen worked with a bigger study population, analyzing data from 7,417 adults in the National Health and Nutrition Examination Survey (NHANES) III and 6,072 adults and children 3 and older in NHANES 1999-2000.
“H. pylori was consistently positively related to HbA1c level in adults, a valid and reliable biomarker for long-term blood glucose levels,” they wrote.
In an editorial appearing in the same issue of the journal, lead author Dani Cohen, an epidemiologist at Tel Aviv University in Israel, suggested that the new findings could have important implications for diabetes prevention and control.
Cohen, a specialist in H. pylori’s health effects, said the next step should be conducting rigorous studies to examine the impact of H. pylori treatment on A1c levels and on the development of diabetes among older adults carrying excess pounds.
http://www.12newsnow.com/story/17156233/diabetes-linked-to-ulcer-causing-bacteria