By Richard Schiffman
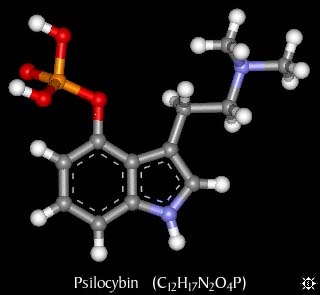
In one of the largest and most rigorous clinical investigations of psychedelic drugs to date, researchers at Johns Hopkins University and New York University have found that a single dose of psilocybin—the psychoactive compound in “magic” mushrooms—substantially diminished depression and anxiety in patients with advanced cancer.
Psychedelics were the subject of a flurry of serious medical research in the 1960s, when many scientists believed some of the mind-bending compounds held tremendous therapeutic promise for treating a number of conditions including severe mental health problems and alcohol addiction. But flamboyant Harvard psychology professor Timothy Leary—one of the top scientists involved—started aggressively promoting LSD as a consciousness expansion tool for the masses, and the youth counterculture movement answered the call in a big way. Leary lost his job and eventually became an international fugitive. Virtually all legal research on psychedelics shuddered to a halt when federal drug policies hardened in the 1970s.
The decades-long research blackout ended in 1999 when Roland Griffiths of Johns Hopkins was among the first to initiate a new series of studies on psilocybin. Griffiths has been called the grandfather of the current psychedelics research renaissance, and a 21st-century pioneer in the field—but the soft-spoken investigator is no activist or shaman/showman in the mold of Leary. He’s a scientifically cautious clinical pharmacologist and author of more than 300 studies on mood-altering substances from coffee to ketamine.
Much of Griffiths’ fascination with psychedelics stems from his own mindfulness meditation practice, which he says sparked his interest in altered states of consciousness. When he started administering psilocybin to volunteers for his research, he was stunned that more than two-thirds of the participants rated their psychedelic journey one of the most important experiences of their lives.
Griffiths believes that psychedelics are not just tools for exploring the far reaches of the human mind. He says they show remarkable potential for treating conditions ranging from drug and alcohol dependence to depression and post-traumatic stress disorder.
They may also help relieve one of humanity’s cruelest agonies: the angst that stems from facing the inevitability of death. In research conducted collaboratively by Griffiths and Stephen Ross, clinical director of the NYU Langone Center of Excellence on Addiction, 80 patients with life-threatening cancer in Baltimore and New York City were given laboratory-synthesized psilocybin in a carefully monitored setting, and in conjunction with limited psychological counseling. More than three-quarters reported significant relief from depression and anxiety—improvements that remained during a follow-up survey conducted six months after taking the compound, according to the double-blind study published December 1 in The Journal of Psychopharmacology.
“It is simply unprecedented in psychiatry that a single dose of a medicine produces these kinds of dramatic and enduring results,” Ross says. He and Griffiths acknowledge that psychedelics may never be available on the drugstore shelf. But the scientists do envision a promising future for these substances in controlled clinical use. In a wide-ranging interview, Griffiths told Scientific American about the cancer study and his other work with psychedelics—a field that he says could eventually contribute to helping ensure our survival as a species.
[An edited transcript of the interview follows.]
What were your concerns going into the cancer study?
The volunteers came to us often highly stressed and demoralized by their illness and the often-grueling medical treatment. I felt very cautious at first, wondering if this might not re-wound people dealing with the painful questions of death and dying. How do we know that this kind of experience with this disorienting compound wouldn’t exacerbate that? It turns out that it doesn’t. It does just the opposite. The experience appears to be deeply meaningful spiritually and personally, and very healing in the context of people’s understanding of their illness and how they manage that going forward.
Could you describe your procedure?
We spent at least eight hours talking to people about their cancer, their anxiety, their concerns and so on to develop good rapport with them before the trial. During the sessions there was no specific psychological intervention—we were just inviting people to lie on the couch and explore their own inner experience.
What did your research subjects tell you about that experience?
There is something about the core of this experience that opens people up to the great mystery of what it is that we don’t know. It is not that everybody comes out of it and says, ‘Oh, now I believe in life after death.’ That needn’t be the case at all. But the psilocybin experience enables a sense of deeper meaning, and an understanding that in the largest frame everything is fine and that there is nothing to be fearful of. There is a buoyancy that comes of that which is quite remarkable. To see people who are so beaten down by this illness, and they start actually providing reassurance to the people who love them most, telling them ‘it is all okay and there is no need to worry’— when a dying person can provide that type of clarity for their caretakers, even we researchers are left with a sense of wonder.
Was this positive result universal?
We found that the response was dose-specific. The larger dose created a much larger response than the lower dose. We also found that the occurrence of mystical-type experiences is positively correlated with positive outcomes: Those who underwent them were more likely to have enduring, large-magnitude changes in depression and anxiety.
Did any of your volunteers experience difficulties?
There are potential risks associated with these compounds. We can protect against a lot of those risks, it seems, through the screening and preparation procedure in our medical setting. About 30 percent of our people reported some fear or discomfort arising sometime during the experience. If individuals are anxious, then we might say a few words, or hold their hand. It is really just grounding them in consensual reality, reminding them that they have taken psilocybin, that everything is going to be alright. Very often these short-lived experiences of psychological challenge can be cathartic and serve as doorways into personal meaning and transcendence—but not always.
Where do you go from here?
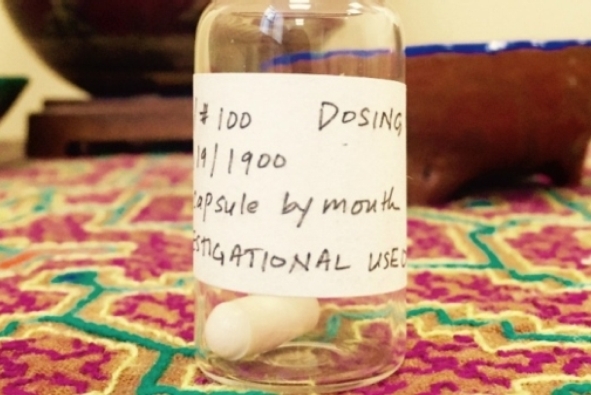
The Heffter Research Institute, which funded our study, has just opened a dialogue with the FDA (Food and Drug Administration) about initiating a phase 3 investigation. A phase 3 clinical trial is the gold standard for determining whether something is clinically efficacious and meets the standards that are necessary for it to be released as a pharmaceutical. Approval would be under very narrow and restrictive conditions initially. The drug might be controlled by a central pharmacy, which sends it to clinics that are authorized to administer psilocybin in this therapeutic context. So this is not writing a prescription and taking it home. The analogy would be more like an anesthetic being dispensed and managed by an anesthesiologist.
You are also currently conducting research on psilocybin and smoking.
We are using psilocybin in conjunction with cognitive behavioral therapy with cigarette smokers to see if these deeply meaningful experiences that can happen with psilocybin can be linked with the intention and commitment to quit smoking, among people who have failed repeatedly to do so. Earlier we ran an uncontrolled pilot study on that in 50 volunteers, in which we had 80 percent abstinence rates at six months. Now we are doing a controlled clinical trial in that population.
How do you account for your remarkable initial results?
People who have taken psilocybin appear to have more confidence in their ability to change their own behavior and to manage their addictions. Prior to this experience, quite often the individual feels that they have no freedom relative to their addiction, that they are hooked and they don’t have the capacity to change. But after an experience of this sort—which is like backing up and seeing the larger picture—they begin to ask themselves ‘Why would I think that I couldn’t stop cigarette smoking? Why would I think that this craving is so compelling that I have to give in to it?’ When the psilocybin is coupled with cognitive behavioral therapy, which is giving smokers tools and a framework to work on this, it appears to be very helpful.
You are also working with meditation practitioners. Are they having similar experiences?
We have done an unpublished study with beginning meditators. We found that psilocybin potentiates their engagement with their spiritual practice, and it appears to boost dispositional characteristics like gratitude, compassion, altruism, sensitivity to others and forgiveness. We were interested in whether the psilocybin used in conjunction with meditation could create sustained changes in people that were of social value. And that appears to be the case.
So it is actually changing personality?
Yes. That is really interesting because personality is considered to be a fixed characteristic; it is generally thought to be locked down in an individual by their early twenties. And yet here we are seeing significant increases in their “openness” and other pro-social dimensions of personality, which are also correlated with creativity, so this is truly surprising.
Do we know what is actually happening in the brain?
We are doing neuro-imaging studies. Dr. Robin Carhart-Harris’s group at Imperial College in London is also doing neuro-imaging studies. So it is an area of very active investigation. The effects are perhaps explained, at least initially, by changes in something [in the brain] called “the default mode network,” which is involved in self-referential processing [and in sustaining our sense of ego]. It turns out that this network is hyperactive in depression. Interestingly, in meditation it becomes quiescent, and also with psilocybin it becomes quiescent. This may correlate with the experience of clarity of coming into the present moment.
That is perhaps an explanation of the acute effects, but the enduring effects are much less clear, and I don’t think that we have a good handle on that at all. Undoubtedly it is going to be much more complex than just the default mode network, because of the vast interconnectedness of brain function.
What are the practical implications of this kind of neurological and therapeutic knowledge of psychedelics?
Ultimately it is not really about psychedelics. Science is going to take it beyond psychedelics when we start understanding the brain mechanisms underlying this and begin harnessing these for the benefit of humankind.
The core mystical experience is one of the interconnectedness of all people and things, the awareness that we are all in this together. It is precisely the lack of this sense of mutual caretaking that puts our species at risk right now, with climate change and the development of weaponry that can destroy life on the planet. So the answer is not that everybody needs to take psychedelics. It is to understand what mechanisms maximize these kinds of experiences, and to learn how to harness them so that we don’t end up annihilating ourselves.
https://www.scientificamerican.com/article/psilocybin-a-journey-beyond-the-fear-of-death/