A woman wearing men’s clothing and claiming to talk directly with God wouldn’t seem to be committing capital crimes.
But in the 15th century, she certainly would have been.
These offenses play a part in the legendary history of Joan of Arc, the teenage heroine who led giant armies to fight against the English during the Hundred Years’ War. She was eventually captured, tried for her crimes, and burned at the stake at the age of 19.
But in modern times, would she be convicted of her crimes on the basis of an insanity plea?

According to a jury of about 200 physicians, forensic psychologists, lawyers, judges, and medical students, the future saint would have been acquitted.
Apparently, having visions of other saints is a sign of mental instability, not heresy.
“She was not mentally responsible for what she had done, as in she was delusional,” Dr. Philip A. Mackowiak, a Carolyn Frenkil and Selvin Passen History of Medicine Scholar-in-Residence at the University of Maryland School of Medicine.
Mackowiak founded the Historical Clinicopathological Conference, held this year at the University of Maryland School of Medicine’s Davidge Hall, the oldest medical facility in the country continuously used for medical education. While similar groups meet to discuss current cases at the university, every year they choose one historic case to dig into.
In 24 years, they’ve covered cases including Beethoven (syphilis), Florence Nightingale (bipolar disorder with psychotic features), Christopher Columbus (HLA-B27-related reactive arthritis), and Charles Darwin (cyclic vomiting syndrome).
At this year’s conference, held last week, they dug into a case memorialized in tempera paint and currently hanging in the Museum of Modern Art in New York.
What Disease Shaped ‘Christina’s World?’
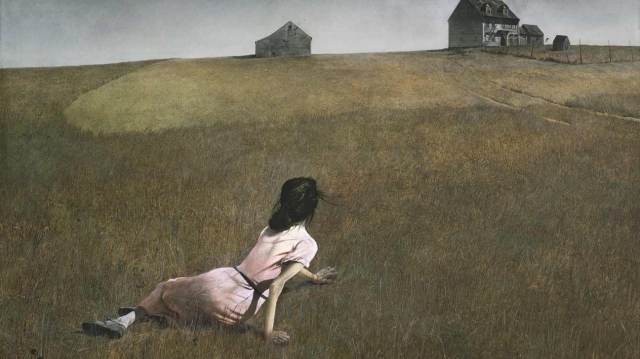
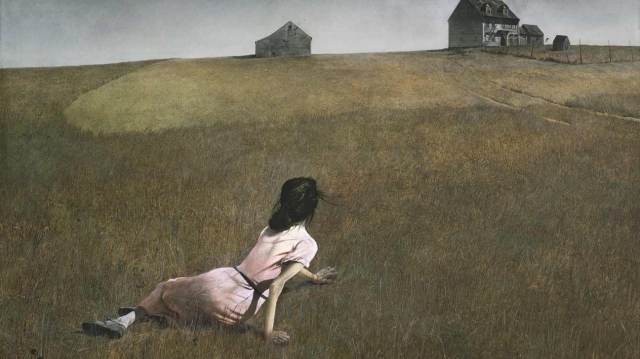
In Andrew Wyeth’s 1948 painting “Christina’s World,” a woman lies in an open field looking toward a house in the distance.
The woman depicted in the painting, Anna Christina Olson, was a friend of Wyeth. She suffered from a mysterious disorder that slowly degraded her ability to walk, so she’d make her way around the grounds by pulling herself along with her hands.
She was later confined to a wheelchair and died in 1968 at the age of 74.
What exactly was the cause of her symptoms?
Charcot-Marie-Tooth disease (CMT), according to Mayo Clinic neurologist Marc Patterson.
CMT, named after the doctors who discovered it, is a group of inherited disorders that affect the peripheral nerves, causing symptoms that include loss of muscle and fine motor skills. It remains incurable and one of the most common inherited neurological disorders.
To reach his diagnosis, Patterson reviewed not only the painting but also what was available of Olson’s medical records from what little biographical information her nieces wrote about her.
“This was a fascinating case,” Patterson said in a press release. “This painting has long been a favorite of mine, and the question of Christina’s ailment was an intriguing medical mystery. I think her case best fits the profile of this disease.”
Piecing Together Historical Health Records
Besides Patterson and the rest of the conference’s expertise, the symptoms were checked using a super computer located at Oak Ridge Leadership Computing Facility, which confirmed the diagnosis.
It also affirmed the previous year’s case, Oliver Cromwell, the English monarch who died in 1658. His undoing was a combination of malaria and typhoid fever caused by a salmonella infection.
Mackowiak takes pride in selecting the case and keeping it under an air of mystery before each year’s conference. The cases are often given vague titles, yet he says most people figure it out before they convene.
Beethoven was “The Sound That Failed,” and Alexander the Great was “Death of a Deity.”
Who was “The Greatest Tragedy in the History of Music?”
No, not Prince, David Bowie, or even John Lennon. It was Mozart, who died of acute rheumatic fever.
Another part of the mystery is that these historical House M.D.s rarely have full autopsy reports or even a single medical record for their subjects, so there is quite a bit of detective work. That only adds to the fun.
In the case of Booker T. Washington, researchers found his great-grandson, who is a physician and helped find Washington’s great-granddaughter. She gave them access to his medical records.
While syphilis was first suspected as a potential cause of death, a blood test done at Rockefeller Hospital in New York City tested negative.
In 2006, the clinicopathological conference determined the slave-turned-advisor to the president died of nephrosclerosis and hypertensive cardiomyopathy. In other words, the man worked his heart to death.
Other cases had to be decided on what was written in the legends.
In the case of Pericles, dubbed “the first citizen of Athens,” researchers went off of descriptions of what happened during the plague that also claimed his sons and first wife.
“To say we provide shocking new information would be an exaggeration,” Mackowiak said.
Mackowiak provides more information on these cases in his two books, “Post-Mortem: Solving History’s Great Medical Mysteries” and “Diagnosing Giants: Solving the Medical Mysteries of Thirteen Patients Who Changed the World.”
For him, every case, every conference meeting highlights how although doctors believe what they’re doing right now is correct, their grandchildren and great-grandchildren will look back and see how wrong they were.
“There is no perfect knowledge,” Mackowiak said. “You do the best with what you have.”
http://www.healthline.com/health-news/medical-researchers-solve-historic-deaths#6