Moments before her planned cesarean delivery last year Gerri Wolfe scrubbed up and donned surgical gloves.
She took her place on the surgical table and her doctors delivered an anesthetic into her spine.
When her surgeon gave her the signal, she reached down and helped deliver her own twin babies. Seconds after they entered the world, she was holding them close to her chest.
In a maternal-assisted cesarean, Mom doesn’t have to miss out on a thing.
Wolfe’s experience wasn’t an isolated case.
Other mothers in Australia have also participated in their cesarean deliveries.
In fact, the Western Australia Department of Health provides guidelines for mother-assisted elective cesarean.
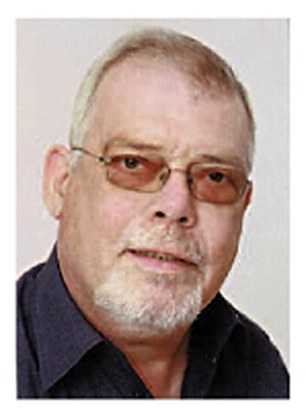
Dr. David Garfinkel, OB-GYN, is an attending physician at Morristown Medical Center in Morristown, New Jersey, and senior partner at One to One FemaleCare. Healthline asked if he has had requests for mother-assisted cesarean delivery.
“I have not been asked to do that, but I would be open to it so long as I could ensure a safe and sterile environment,” he said. “There is a special system (drapes and sterile gloves for the mother) that can help facilitate that request. Safety is number one in providing care for the mother and the newborn.”
In the first half of the 20th century, control over how women gave birth went from mothers and midwives to doctors and hospitals.
By the 1960s, there was a growing movement to turn that around again. Moms wanted to be awake and alert. They also wanted fathers and partners to be able to share the experience.
Today, mothers-to-be work with their doctors, midwives, and support systems to create a personalized childbirth experience.
When you’re planning for a cesarean delivery, it’s an entirely different story.
While some cesarean deliveries are emergencies, many are planned ahead of time. Among the reasons for this are multiple births, large babies, or maternal health conditions that complicate labor and delivery.
In the United States, the cesarean delivery rate is slightly more than 32 percent of all births, according to the Centers for Disease Control and Prevention (CDC).
It’s a common procedure, but that doesn’t make it a minor one. A planned cesarean delivery is generally performed using an epidural so the mother can stay awake but not feel the pain of surgery.
A small curtain prevents the mother from seeing her own abdomen get cut open. It also prevents her from seeing her newborn enter the world.
Some mothers and doctors want to change that.
Mother-assisted cesarean delivery may not be all the rage in the United States, but there is a movement toward friendlier cesarean birth.
“A gentle C-section is a change in the attitudes toward C-sections,” said Garfinkel. “It’s where the care team (the OB, anesthesiologists, and nurse) aims to make the C-section experience in the operating room as similar as possible to the labor and delivery room.”
Garfinkel explained that with a gentle C-section, there are no drapes to block the woman’s view.
“While the patient may not be pushing, a patient can see the baby entering into the world for the first time. Unlike a traditional C-section, where the baby and partner are taken out of the room, a gentle C-section allows the family to stay together in one room, with the baby being cared for in the same room as the mother,” he said.
How women give birth has been evolving for decades. Now some are assisting in their own cesarean deliveries.
women watching c-sections
Moments before her planned cesarean delivery last year Gerri Wolfe scrubbed up and donned surgical gloves.
She took her place on the surgical table and her doctors delivered an anesthetic into her spine.
When her surgeon gave her the signal, she reached down and helped deliver her own twin babies. Seconds after they entered the world, she was holding them close to her chest.
In a maternal-assisted cesarean, Mom doesn’t have to miss out on a thing.
I have not been asked to do that, but I would be open to it so long as I could ensure a safe and sterile environment.
Dr. David Garfinkel, Morristown Medical Center
Wolfe’s experience wasn’t an isolated case.
Other mothers in Australia have also participated in their cesarean deliveries.
In fact, the Western Australia Department of Health provides guidelines for mother-assisted elective cesarean.
Dr. David Garfinkel, OB-GYN, is an attending physician at Morristown Medical Center in Morristown, New Jersey, and senior partner at One to One FemaleCare. Healthline asked if he has had requests for mother-assisted cesarean delivery.
“I have not been asked to do that, but I would be open to it so long as I could ensure a safe and sterile environment,” he said. “There is a special system (drapes and sterile gloves for the mother) that can help facilitate that request. Safety is number one in providing care for the mother and the newborn.”
Read More: Cesarean Rates Starting to Drop in the United States »
Changing Attitudes About Childbirth
In the first half of the 20th century, control over how women gave birth went from mothers and midwives to doctors and hospitals.
By the 1960s, there was a growing movement to turn that around again. Moms wanted to be awake and alert. They also wanted fathers and partners to be able to share the experience.
Today, mothers-to-be work with their doctors, midwives, and support systems to create a personalized childbirth experience.
When you’re planning for a cesarean delivery, it’s an entirely different story.
women watching c-sections
While some cesarean deliveries are emergencies, many are planned ahead of time. Among the reasons for this are multiple births, large babies, or maternal health conditions that complicate labor and delivery.
In the United States, the cesarean delivery rate is slightly more than 32 percent of all births, according to the Centers for Disease Control and Prevention (CDC).
It’s a common procedure, but that doesn’t make it a minor one. A planned cesarean delivery is generally performed using an epidural so the mother can stay awake but not feel the pain of surgery.
A small curtain prevents the mother from seeing her own abdomen get cut open. It also prevents her from seeing her newborn enter the world.
Some mothers and doctors want to change that.
Read More: A Mother’s Journey Through Chemotherapy and Pregnancy »
The ‘Gentle C-Section’
Mother-assisted cesarean delivery may not be all the rage in the United States, but there is a movement toward friendlier cesarean birth.
“A gentle C-section is a change in the attitudes toward C-sections,” said Garfinkel. “It’s where the care team (the OB, anesthesiologists, and nurse) aims to make the C-section experience in the operating room as similar as possible to the labor and delivery room.”
Garfinkel explained that with a gentle C-section, there are no drapes to block the woman’s view.
“While the patient may not be pushing, a patient can see the baby entering into the world for the first time. Unlike a traditional C-section, where the baby and partner are taken out of the room, a gentle C-section allows the family to stay together in one room, with the baby being cared for in the same room as the mother,” he said.
The gentle C-section allows immediate skin-to-skin contact or breastfeeding.
More patients at his facility are asking about them, said Garfinkel. He believes gentle C-sections are the future.
Besides the mother, this type of cesarean delivery benefits the father or partner and allows family bonding time.
The experience may feel gentler, but Garfinkel makes it clear that it’s still major surgery.
“As a physician, I am not being more gentle as I do the surgery,” he said.
He performs gentle C-sections, but Garfinkel has no interest in increasing the rate of cesarean births unnecessarily. He and his practice promote vaginal births whenever possible.
But if a cesarean delivery is called for, he wants his patients to have the option of a gentler, more emotional experience.
“A gentle C-section allows a woman to be almost as involved as if her birth was happening vaginally,” he said. “I believe all women should be given the opportunity to be as much a part of their births as they want.”
For those who are interested in pursuing a gentle C-section, Garfinkel recommends interviewing providers and asking about their attitudes toward these types of deliveries well in advance of the due date.
http://www.healthline.com/health-news/women-who-want-to-watch-their-c-sections#5