By DAVE PHILIPPS
After three tours in Iraq and Afghanistan, C. J. Hardin wound up hiding from the world in a backwoods cabin in North Carolina. Divorced, alcoholic and at times suicidal, he had tried almost all the accepted treatments for post-traumatic stress disorder: psychotherapy, group therapy and nearly a dozen different medications.
“Nothing worked for me, so I put aside the idea that I could get better,” said Mr. Hardin, 37. “I just pretty much became a hermit in my cabin and never went out.”
Then, in 2013, he joined a small drug trial testing whether PTSD could be treated with MDMA, the illegal party drug better known as Ecstasy.
“It changed my life,” he said in a recent interview in the bright, airy living room of the suburban ranch house here, where he now lives while going to college and working as an airplane mechanic. “It allowed me to see my trauma without fear or hesitation and finally process things and move forward.”
Based on promising results like Mr. Hardin’s, the Food and Drug Administration gave permission Tuesday for large-scale, Phase 3 clinical trials of the drug — a final step before the possible approval of Ecstasy as a prescription drug.
If successful, the trials could turn an illicit street substance into a potent treatment for PTSD.
Through a spokeswoman, the F.D.A. declined to comment, citing regulations that prohibit disclosing information about drugs that are being developed.
“I’m cautious but hopeful,” said Dr. Charles R. Marmar, the head of psychiatry at New York University’s Langone School of Medicine, a leading PTSD researcher who was not involved in the study. “If they can keep getting good results, it will be of great use. PTSD can be very hard to treat. Our best therapies right now don’t help 30 to 40 percent of people. So we need more options.”
But he expressed concern about the potential for abuse. “It’s a feel-good drug, and we know people are prone to abuse it,” he said. “Prolonged use can lead to serious damage to the brain.”
The Multidisciplinary Association for Psychedelic Studies, a small nonprofit created in 1985 to advocate the legal medical use of MDMA, LSD, marijuana and other banned drugs, sponsored six Phase 2 studies treating a total of 130 PTSD patients with the stimulant. It will also fund the Phase 3 research, which will include at least 230 patients.
Two trials here in Charleston focused on treating combat veterans, sexual assault victims, and police and firefighters with PTSD who had not responded to traditional prescription drugs or psychotherapy. Patients had, on average, struggled with symptoms for 17 years.
After three doses of MDMA administered under a psychiatrist’s guidance, the patients reported a 56 percent decrease of severity of symptoms on average, one study found. By the end of the study, two-thirds no longer met the criteria for having PTSD. Follow-up examinations found that improvements lasted more than a year after therapy.
“We can sometimes see this kind of remarkable improvement in traditional psychotherapy, but it can take years, if it happens at all,” said Dr. Michael C. Mithoefer, the psychiatrist who conducted the trials here. “We think it works as a catalyst that speeds the natural healing process.”
The researchers are so optimistic that they have applied for so-called breakthrough therapy status with the Food and Drug Administration, which would speed the approval process. If approved, the drug could be available by 2021.
Under the researchers’ proposal for approval, the drug would be used a limited number of times in the presence of trained psychotherapists as part of a broader course of therapy. But even in those controlled circumstances, some scientists worry that approval as a therapy could encourage more illegal recreational use.
“It sends the message that this drug will help you solve your problems, when often it just creates problems,” said Andrew Parrott, a psychologist at Swansea University in Wales who has studied the brains of chronic Ecstasy users. “This is a messy drug we know can do damage.”
Allowing doctors to administer the drug to treat a disorder, he warned, could inadvertently lead to a wave of abuse similar to the current opioid crisis.
During initial studies, patients went through 12 weeks of psychotherapy, including three eight-hour sessions in which they took MDMA. During the sessions, they lay on a futon amid candles and fresh flowers, listening to soothing music.
Dr. Mithoefer and his wife, Ann Mithoefer, and often their portly terrier mix, Flynn, sat with each patient, guiding them through traumatic memories.
“The medicine allows them to look at things from a different place and reclassify them,” said Ms. Mithoefer, a psychiatric nurse. “Honestly, we don’t have to do much. Each person has an innate ability to heal. We just create the right conditions.”
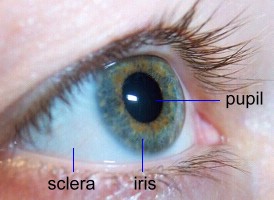
Research has shown that the drug causes the brain to release a flood of hormones and neurotransmitters that evoke feelings of trust, love and well-being, while also muting fear and negative emotional memories that can be overpowering in patients with post-traumatic stress disorder. Patients say the drug gave them heightened clarity and ability to address their problems.
For years after his combat deployments, Mr. Hardin said he was sleepless and on edge. His dreams were marked with explosions and death. The Army gave him sleeping pills and antidepressants. When they didn’t work, he turned to alcohol and began withdrawing from the world.
“I just felt hopeless and in the dark,” he said. “But the MDMA sessions showed me a light I could move toward. Now I’m out of the darkness and the world is all around me.”
Since the trial, he has gone back to school and remarried.
The chemist Alexander Shulgin first realized the euphoria-inducing traits of MDMA in the 1970s, and introduced it to psychologists he knew. Under the nickname Adam, thousands of psychologists began to use it as an aid for therapy sessions. Some researchers at the time thought the drug could be helpful for anxiety disorders, including PTSD, but before formal clinical trails could start, Adam spread to dance clubs and college campuses under the name Ecstasy, and in 1985, the Drug Enforcement Administration made it a Schedule 1 drug, barring all legal use.
Since then, the number of people seeking treatment for PTSD has exploded and psychiatry has struggled to keep pace. Two drugs approved for treating the disorder worked only mildly better than placebos in trials. Current psychotherapy approaches are often slow and many patients drop out when they don’t see results. Studies have shown combat veterans are particularly hard to treat.
In interviews, study participants said MDMA therapy had not only helped them with painful memories, but also had helped them stop abusing alcohol and other drugs and put their lives back together.
On a recent evening, Edward Thompson, a former firefighter, tucked his twin 4-year-old girls into bed, turned on their night light, then joined his wife at a backyard fire.
“If it weren’t for MDMA … ” he said.
“He’d be dead,” his wife, Laura, finished.
They both nodded.
Years of responding to gory accidents left Mr. Thompson, 30, in a near constant state of panic that he had tried to numb with alcohol and prescription opiates and benzodiazepines.
By 2015, efforts at therapy had failed, and so had several family interventions. His wife had left with their children, and he was considering jumping in front of a bus.
A member of a conservative Anglican church, Mr. Thompson had never used illegal drugs. But he was struggling with addiction from his prescription drugs, so he at first rejected a suggestion by his therapist that he enter the study. “In the end, I was out of choices,” he said.
Three sessions with the drug gave him the clarity, he said, to identify his problems and begin to work through them. He does not wish to take the drug again.
“It gave me my life back, but it wasn’t a party drug,” he said. “It was a lot of work.”