Conor Liston, Professor of Psychiatry at Weill Cornell Medicine, and senior author of the study.
September 6, 2024
Depression doesn’t mean you’re always feeling low. Sure, most times it’s hard to crawl out of bed or get motivated. Once in a while, however, you feel a spark of your old self—only to get sucked back into an emotional black hole.
There’s a reason for this variability. Depression changes brain connections, even when the person is feeling okay at the moment. Scientists have long tried to map these alternate networks. But traditional brain mapping technologies average multiple brains, which doesn’t capture individual brain changes.
This week, an international team took a peek into the depressed mind. With brain imaging technology called precision functional mapping, they captured the brains of 135 people with depression for over a year and a half.
The largest brain mapping study of the disorder to date, the results revealed a curious change in the brain’s connections in people with depression—a neural network, usually involved in attention, nearly doubled its size compared to those without the condition. The increase remained even during periods when the person no longer felt low.
The brain signature isn’t just a neurobiological sign of depression—it could also be a predictor. When observed in the brain imaging data of nearly 12,000 children starting from nine years old, the expanded network predicted the onset of depression later in adolescence.
So far, brain imaging studies for depression have been “one size fits all,” in that studies compare averaged brain scans between people with or without depression, explained the team in their study.
With precision functional mapping, it’s possible to track individual brain trajectories as they change over time. In turn, this could lead to more nuanced insights into neural connections in depression and inspire more sophisticated and personalized brain implants to tackle the disorder.
To Dr. Caterina Gratton at the University of Illinois Urbana-Champaign, who was not involved in the work, the precise details from the brain scans are impressive. “Rather than reading a few pages of many books, we’re reading whole chapters,” she told Nature.
The Old Playbook
Scientists have long tried to decipher the brain networks underlying depression.
There have been successes. At the turn of this century, neurologist Dr. Helen Mayberg and colleagues spearheaded brain mapping studies that compared brains with the disorders and those without. They eventually pinpointed a region at the front of brain that hyperactivates in people with severe depression.
Given deep brain stimulation in the region—a technique where implanted electrodes zap dysfunctional circuits with brief pulses of electricity—some patients rapidly improved. Since then, neuroscientists have identified multiple brain networks involved in the disorder. However, larger trials of deep brain stimulation yielded mixed results.
Some patients didn’t respond to the treatment. But others experienced life-altering changes. In 2021, a woman named Sarah received a personalized brain implant. She had battled severe depression for years and had tried a range of medications. None of them worked. But the implant did. Fine-tuned to her brain’s unique electrical signals, for the first time in her life, Sarah had her depression under control. “I’m finally laughing,” she said at the time.
Sarah’s case highlighted two points for tackling the brain networks involved in depression. One, the disorder affects each brain differently. And two, depression is chronic, with ebbs and flows in mood. Imaging brain connection changes at just one point in time isn’t enough—what’s needed is to follow the brain’s functional changes over time.
Precision Mapping
There are many ways to track brain function, but a popular one is functional magnetic resonance imaging (fMRI). The technology tracks changes in blood flow in the brain—a proxy for activity—and builds a map of how different regions and brain connections “talk” to each other.
But our brains are snowflakes. Although brain networks look similar on average, each person slightly deviates. Precision mapping captures these individual differences, with previous studies showing that the size, shape, and location of neural networks can markedly differ, but are generally stable for each person. In other words, we all have a unique “brainprint.”
However, depression changes these dynamics as the disorder progresses. A single fMRI brain scan—a snapshot—can’t capture the brain’s trajectory over time.
The team tackled these problems head-on. In a first small study, they repeatedly imaged the brains of 6 people with depression—ranging from mild to severe—across 22 sessions. Precision mapping was also used for 37 people without the disorder.
By looking at brain activation patterns, “it was immediately apparent” that a brain network changed in people with depression, even without averaging the results. Dubbed the “salience network,” it relies on multiple brain regions to help us navigate the world with purpose. The network combines outside stimulation with an internal goal—say, make a cup of coffee for an early morning jolt. As a central networking hub in the brain, it lets us decide what to pay attention to.
In people with depression, the network expanded twice as much, compared to controls—in that more parts of the brain activated to support it.
Six people hardly represent the entire spectrum of depression. To validate their findings, the team turned to three existing datasets from Weill Cornell Medicine and Stanford University. Totaling 135 people with depression, the datasets captured detailed brain images and demographic and clinical information. Almost every person with depression showed a larger salience network. They also saw a similar brain pattern in an additional dataset of nearly 300 people with depression, who didn’t respond to antidepressant drugs.
Symptoms of depression ebb and flow. Does network expansion follow the pattern? In another test, they used precision fMRI to follow people with depression roughly every week for up to a year and a half. With each scan, the participants also reported their mood based on a standardized depression scale.
Regardless of current emotions, the salience network remained roughly the same size for each person. However, the strength of connections between the network’s components changed—decreasing when the person was actively depressed. Using AI to analyze these patterns, the team was able to predict—for any of the participants—if they might experience a depressive episode the following week.
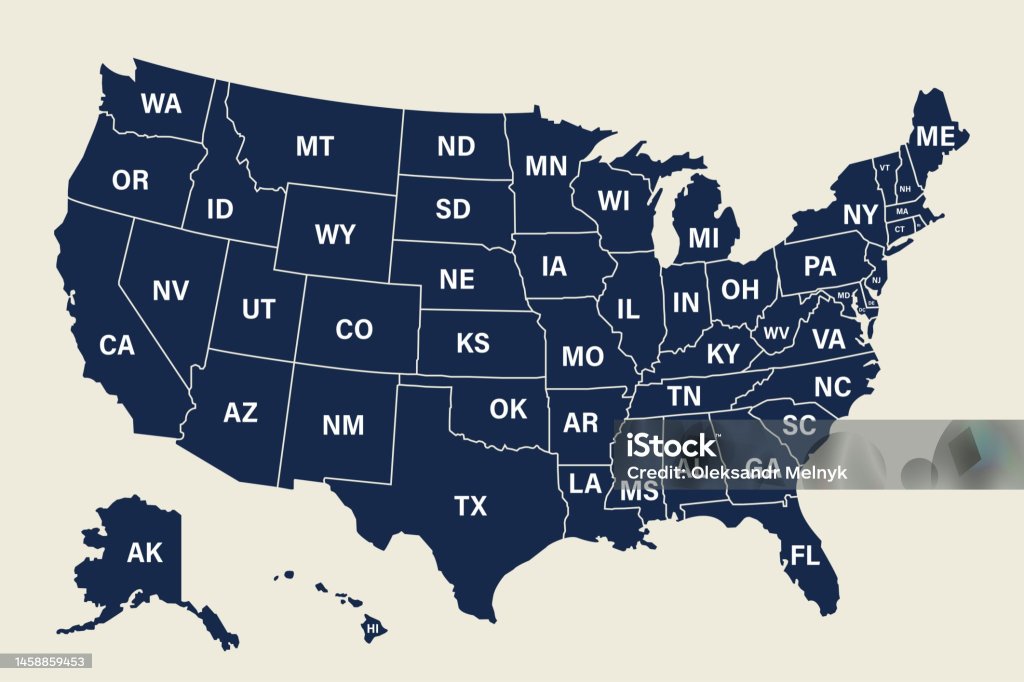
The results suggest that an expanded salience network, and its inner connections, isn’t just a marker for depression after symptoms have already set in. It could also be a predictor. To test the idea, they tapped into the Adolescent Brain Cognitive Development (ABCD) dataset, the largest long-term study of brain development and health for children in the US. The ambitious project tracks nearly 12,000 children across the country, from nine years old to young adulthood.
By analyzing salience network expansion, the team identified 57 kids, aged 10 to 12 years old, who eventually developed depression a few years later. Their salience network was already far larger than similarly aged peers at their initial visit. If replicated in more children, it could be a feature that helps predict depression risk and allows early intervention.
For now, scientists don’t know why or how the network expands. It could be partly due to genetics, which plays a role in depression. Another reason could be the brain dials up the network during depressive episodes, recruiting more brain cells and resulting in the network’s growth. But the study shows the power of precision brain mapping over time.
The results “will open new avenues for understanding cause and effect” when it comes to brain changes and depression, wrote the team, “and for designing personalized, prophylactic treatments.”
https://singularityhub.com/2024/09/06/a-brain-signature-of-depression-revealed-by-new-brain-mapping-study/?utm_campaign=SU%20Hub%20Daily%20Newsletter&utm_medium=email&_hsenc=p2ANqtz–r5z87LpqVZli5XoPpwTeSgPkl3N6QDfraQXW6DMqNgRi3rmbxsNDGUcfJTdxnEnxW0fZZQkES7xoJttQpYh7-MnTpgg&_hsmi=323541798&utm_content=323541798&utm_source=hs_email